

Delusional disorder: a case of jealousy
Gaceta Médica Boliviana, vol.. 43, no. 2, 2020
Universidad Mayor de San Simón


Casos Clinicos
Received: 10 September 2020
Accepted: 05 November 2020

Abstract: Delusional disorder is a rare psychiatric condition characterised by the presence of delusions of erotomania, persecution, jealousy, grandeur and somatic delusions. It has an insidious onset and tends to become chronic, altering behaviour, affecting the individual’s functionality and compromising interpersonal relationships. The etiology is unknown, the diagnosis is made clinically based on DSM-V or ICD-10 criteria and the treatment currently available provides a limited response. In general, patients do not recognise the disorder, do not seek medical attention and have poor adherence to treatment. The clinical case presented is of a middle-aged man with a Delusional Disorder of the celotypic type directed at his wife, which gradually compromises the patient’s quality of life and puts the family at risk; his response to the atypical antipsychotic was partial, but with considerable improvement in family coexistence. The importance of this clinical case lies in the fact that it is a pathology that is not very prevalent and less well known by health professionals or other related disciplines, in addition to the fact that there are no publications in the field on the subject; it is therefore necessary to publicise cases like this, providing information for early diagnosis with timely treatment, in order to improve the long-term prognosis and quality of life of the patient, in addition to preventing criminal behaviour, with possible fatal outcomes.
Keywords: mental disorders, jealousy, domestic violence.
Resumen: El trastorno delirante es un trastorno psiquiátrico poco frecuente y se caracteriza por la presencia de ideas delirantes cuyo contenido puede ser de tipo erotomaníaco, de persecución, celotipia, de grandeza y somática. Tiene un inicio insidioso y tiende a la cronicidad, altera la conducta, repercute en la funcionalidad del individuo y compromete sus relaciones interpersonales. La etiología es desconocida, el diagnóstico se realiza mediante la clínica apoyándose en los criterios del DSM-V o CIE-10 y el tratamiento disponible en la actualidad proporciona una respuesta limitada. En general los pacientes no reconocen el trastorno, no recurren a la atención médica y tienen baja adherencia al tratamiento. El caso clínico que se expone es de un hombre de mediana edad que presenta un Trastorno Delirante tipo celotípico dirigido a su esposa y que gradualmente compromete la calidad de vida del paciente y pone a la familia en riesgo vital; su respuesta al antipsicótico atípico fue parcial, pero con mejoría considerable en la convivencia familiar. La importancia de este caso clínico reside en que es una patología poco prevalente y menos conocida por los profesionales del área de salud u otras disciplinas afines, además que no hay publicaciones en el medio sobre el tema; por lo que es necesario dar a conocer casos como este, proporcionando información para un diagnóstico temprano con tratamiento oportuno, con el fin de mejorar el pronóstico a largo plazo y la calidad de vida del paciente, además de prevenir conductas delictivas, con posibles desenlaces fatales.
Palabras clave: trastorno mental, celos, violencia doméstica.
Delusional disorder (TD) is a psychotic disorder that has as its central axis non-bizarre, systematised, permanent false beliefs related to the individual’s experiences; the delusional construct is a continuity of the patient’s biography and is possible within the individual’s cultural context, with the preservation of the other cognitive spheres1,2.
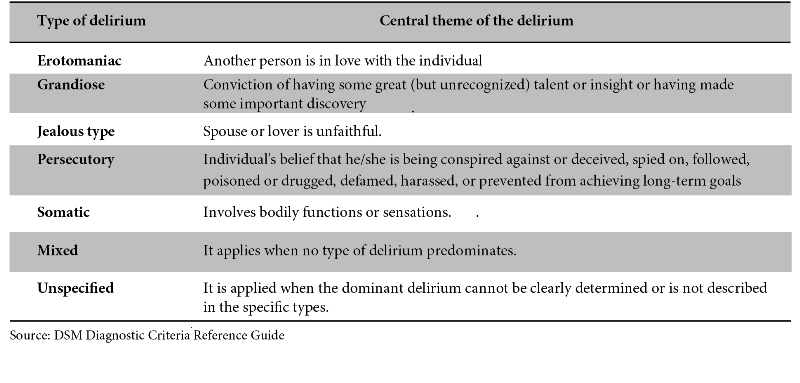
The beliefs may be erotomanic, persecutory, zealotypical, grandiose and somatic, and may clinically present as an isolated subtype, a combination of subtypes with predominance of one, or unspecified, with the presentation of elements of several subtypes) (Table 1)1,2,3.
The first available record mentioning the term delirium and its derivatives was made by Voegel in the 18th century and then Kalbaum in 1863 who describes and names delusions without cognitive impairment as “paranoia”; but it is Kraepelin who introduces the concept of an insidious disease, of endogenous origin, with delusions developing in a susceptible personality through an interpretative mechanism of chronic evolution and with the preservation of other cognitive spheres2;. This conception, to which the contributions of different schools were added, contributed to the construction, conceptualisation and delimitation of the disorder and in 1987, the DSM-III (Diagnostic and Statistical Manual of Mental Disorders, 3rd edition) identified and published TD as a nosological entity independent of schizophrenia, because until that time it was considered a benign or mild manifestation of this disorder1,2,4.
TD is not very prevalent, affecting approximately 0.2% to 0.3% of the general population2 and accounts for 1 to 4% of psychiatric hospital admissions, although it is assumed that this incidence is underestimated due to the low spontaneous attendance of patients at mental health centres2,4.
TD shows differences in its presentation according to sex; it is slightly more prevalent in women (1.2:1), they are generally married or widowed,2,4manifest more frequently the erotomanic subtype1,2,4,5 and present greater functional compromise5. Men present more often with the persecutory subtype, followed by delusions of grandeur and finally zealotypy,1,2,4,5 they are generally single and have better overall functioning than women5.
TD is related to low socioeconomic and educational levels, with 2/3 being illiterate or not having completed primary school6. The literature also mentions sensory deficits, immigration, previous stressful episodes, history of psychotropic substance use, traumatic brain injury, psychosocial factors and family history of psychosis,4,6 isolation and personality characteristics² as risk factors for the development of TD.
The etiology of TD is unknown;2 perceptual abnormalities, motivational factors, information processing deficits and adverse early experiences are hypothesised1,2. Other authors propose different causal factors in the understanding of delusional ideas that would be responsible for the clinical picture, such as preoccupational style of thinking, negative self-beliefs, interpersonal sensitivity, sleep disturbances, abnormal internal experience and biases in reasoning7,8. It has an insidious and chronic character,1,2 so the diagnosis is usually late, when the person is around 40 years old9. Patients arrive at the mental health service forced by their family, referred by another doctor or forced by the courts;2 when they seek medical attention voluntarily, they do so because of the symptoms generated by the delusional ideas: anxiety, insomnia, irritability, physical discomfort, among others, not because of the delusional content itself, because the patient does not believe they are delirious, this being one of the fundamental characteristics for diagnosis10.
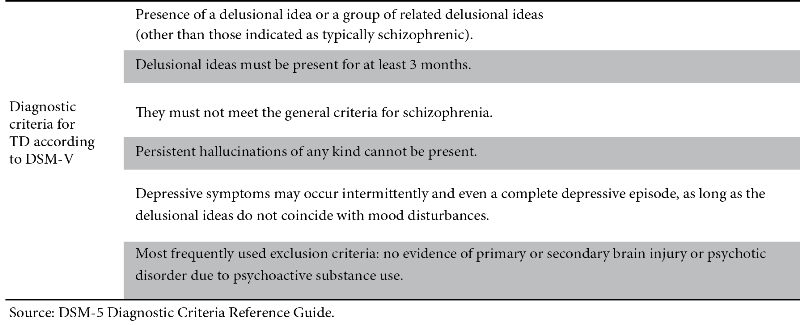
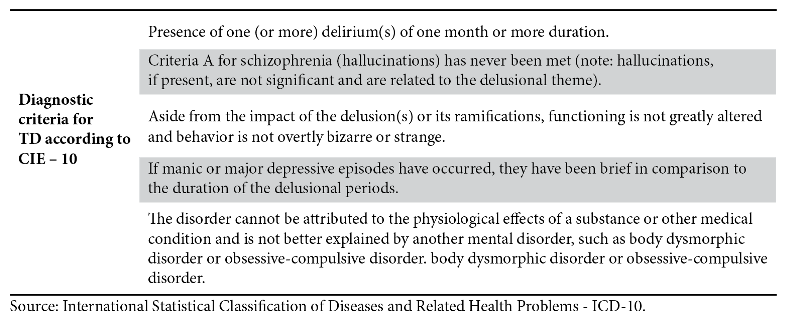
For a diagnosis of this disorder to be made, delusional ideas must be present for at least three consecutive months and affect the individual’s functionality with other cognitive areas (memory, intelligence, attention, etc.) preserved1-3,11. Delusional symptoms may be accompanied by hallucinations, depressed mood or anxiety, but must not meet the diagnostic criteria for other mental disorders such as schizophrenia or mood disorders; nor can the symptoms be attributable to the effect of psychoactive substances, drugs or medical illnesses1-3,11.
Diagnosis is currently clinical1,2 and the diagnostic criteria of the International Code of Diseases, 10th edition (ICD-10) (Table 2) and/or DSM-V (Table 3)1,2 are used as normative support.
Antipsychotics (AP) are the mainstay treatment for TD, providing control of delusions, agitation, anxiety and behavioural disturbances1,2. APs are divided into typical and atypical, according to their mechanism of action, both of which are effective in controlling delusional symptoms, but their use is restricted, especially for typical APs, due to acute adverse effects that are poorly tolerated by patients. Some studies consider atypical APs superior, but this cannot be generalised9 because the studies were conducted with unrepresentative samples. Current alternatives include pimozide - typical AP- which is well tolerated by patients, but is not available in some countries such as Bolivia, risperidone - atypical AP - widely used in TD, with good response and less acute adverse effects; other atypical APs can be used and the choice will depend on the patient’s profile, taking into account comorbidities, tolerance to side effects, the patient’s preferred route of administration, accessibility to medication and availability in the environment.12 In general, patients need other classes of drugs for the control of acute symptoms associated with the central disorder, such as anxiety, insomnia or comorbidities, but they are not the mainstay of treatment for TD.
Treatment presents multiple difficulties such as poor awareness of the disorder by the patient which, associated with frequent side effects, leads to poor adherence and abandonment of pharmacological treatment. Another problem is the resistance of the disorder to currently available drugs, so that symptom control is partial and it is necessary to try different drugs and doses, leading to more mistrust on the part of the patient in relation to their diagnosis12.
Of the psychological therapies, individual psychotherapy is more effective than group therapy, but a relationship of trust between the doctor and the patient is essential, and the initial focus must be diverted towards the anxiety or irritability produced by the situations that generate the delusions;12 in this way, if the patient perceives that their delusions are not the objective of the psychotherapy, better adherence to treatment can be achieved.
Cognitive Behavioural Therapy (CBT) is mentioned in some studies with favourable results, but it cannot be said to be really effective because there is a lack of comparative studies13.
Comorbidities with other psychiatric pathologies are frequent, with mood disorders in women and alcohol and psychoactive substance use in men;4,9 both conditions are associated with greater severity, worse prognosis and higher prevalence of suicidal ideation and attempts6,5,14.
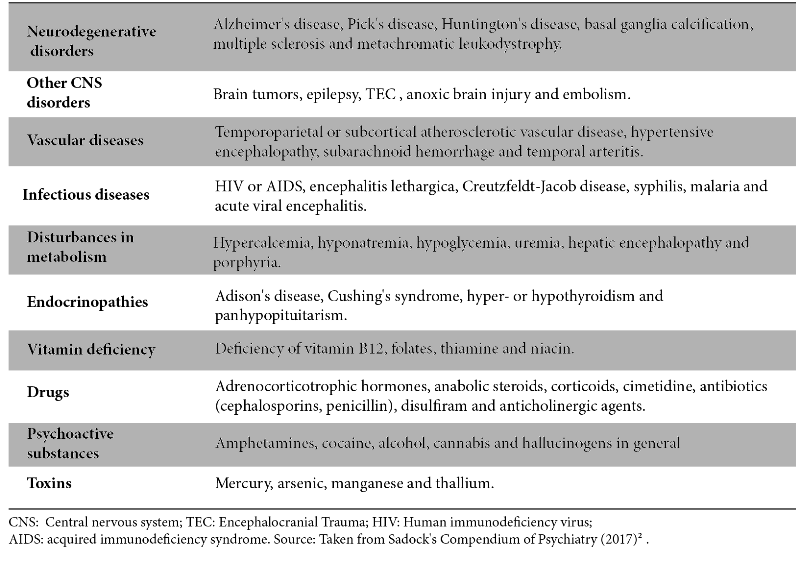
Differential diagnosis should be made with endocrine, metabolic, neurological diseases, acute confusional syndrome and exposure to some drugs or toxic substances (Table IV)1,2,10. In the range of mental illnesses, the differential diagnosis should be made with schizophrenia and mood disorders; and according to the delusional content, with hypochondriacal disorder and paranoid personality disorder10.
The prognosis is guarded, there are few reference studies and they tend not to coincide in relation to the figures; Sadock (2017),2 mentions that 50% of patients recover with long-term follow-up, 20% decrease their symptoms and 30% show no change. Another publication indicates that, under treatment, 50% maintain a continuous clinical course, and 33% show remission. Palomo (2009)1 infers that 42% of patients with treatment maintain good social functioning and 44% manage to maintain their work activity1. Other studies show that 42% of patients with treatment maintain good social functioning and 44% manage to maintain their work activity1.
Factors contributing to a better prognosis are: being female, young (which implies onset of TD before the age of 30), being married, understanding the disorder, being married, understanding the disorder, having a good pre-morbid social and occupational adaptation; acute onset with the presence of precipitating factors, short duration of the episode and immediate and/or progressive response to treatment1,2,10. Among the subtypes, the persecutory, somatic and erotomanic subtypes have the best prognosis and the celotipic subtype the worst2. There are few high quality studies on TD but they were generally conducted in small populations, have several limitations and controversial results.
Presentation of the case
47-year-old man, admitted to the Acute Ward of the San Juan de Dios Psychiatric Institute, after an outpatient evaluation and with an initial diagnosis of Acute Psychotic Disorder, to rule out Delusional Disorder. It was the first time that the patient had attended a mental health center; he was brought against his will by his wife and children, with the support of a nurse specialised in the transfer of patients with mental disorders.
The patient came from a province in the department of Cochabamba, and his childhood was marked by many adverse experiences that culminated in parental abandonment and the beginning of his work at an early age in multiple activities. He did not complete his primary education, but despite the scarcity of resources and lack of support, in adulthood he managed to own several real estate properties and enjoy a comfortable life, currently dedicated to importing vehicles.
He married at the age of 20 and had two children. As personal characteristics, the wife mentions that the patient was reserved, honest, hard-working and distrustful. No relevant personal or family history could be identified, and it was not possible to investigate other data due to the lack of relationship between the patient and his biological family; neither did he have any significant medical or surgical history, except for a right hearing loss as a result of an ear infection in the past. Regarding the consumption of alcohol and psychotropic substances, he drank alcoholic beverages sporadically and he “acullicaba” (a term derived from the Quechua “akullikuy” meaning to chew a bolus of coca leaves) occasionally.
According to the wife, the patient had irrational ideas about his marital fidelity, he engaged in behaviour aimed at constantly proving the alleged adultery, associated with alterations in his behaviour that became violent towards her and his children, whom he accused of being “pimps” for their mother, out of frustration at not being able to prove his hypothesis.
The wife recalled that, since she had known him, the patient had been a jealous man, but she interpreted these displays of jealousy as signs of affection and care. Over time this behaviour progressively intensified and in the last year it became impossible to tolerate; he locked her in her room, prevented her from leaving her own house, made her the victim of physical and psychological aggression, any finding of the patient could be considered as a vestige of his infidelity, making unconnected associations to prove his suppositions. He became suspicious of everyone, with ideas of self-referential harm and persecution related to the primary delusional idea: the wife’s infidelity. He was hyper-alert, anxious, did not sleep at night, started smoking tobacco and increased the amount and frequency of alcoholic beverages and coca leaf smoking. In the last few months, he spent the night in hotels or in the homes of relatives, only returning home during the day, and in order to look for traces to support his suspicion, he abandoned his business and his personal care. It was suggested to him to go to a hospital on more than one occasion, but he flatly refused, stating that he was not ill and that this suggestion was part of a plot to disable him of his faculties and take over his assets together with his wife’s alleged lover. The family’s motivation for taking the patient for psychiatric evaluation was that a relative had alerted them that he had acquired a firearm and that there was a risk that it could be used against his wife or another close relative.
On mental examination on admission, it was noted that the patient had a regular grooming and personal hygiene, was suspicious but was cooperative with the interview, restless, egoistic, speech without alteration in form but in content, of celotypical and persecutory delirious type; he admitted visual and sporadic sensoperceptive alterations related to the content of thought, anxious affect, globally oriented in the three spheres, euproséxico, preserved memory, intelligence with a tendency to concrete thought and without judgement of illness. Physical examination showed moderate bilateral hypoacusis; the other systems were unaltered.
Laboratory results during hospitalisation showed liver, renal and pancreatic function, coagulation, haemogram and urine without alterations. The psychology report showed low normal intelligence (IQ: 80-90) and personality with paranoid traits. During his hospitalisation of approximately two months, he showed a slow but progressive and favourable evolution. On admission, treatment was started with an atypical AP, risperidone at a dose of 1.5 mg/day, reaching 9 mg/day during hospitalisation, in addition to other drugs to regulate the sleep-wake cycle and to control extrapyramidal symptoms that arose when trying to change the medication, levomepromazine and biperidene, respectively; he also received individual and family psychotherapy.
He was discharged from hospital with risperidone at a dose of 6 mg/day, which partially controlled his delusional celotypic symptoms; he was less suspicious and impulsive and reconciled with his family, although the ideas of his wife’s infidelity were still latent, but not active. The patient attended regular check-ups, initially every week, then more and more frequently, becoming monthly; the doses of risperidone were reduced to 3 mg/day, with a good clinical response observed in the reduction of impulsive behaviour, the return to work and a more harmonious family life; Even so, he showed some mistrust of his environment, but did not show delusions and disagreement with the need to take the medication indefinitely, arguing several adverse effects (not consistent with what is reported in the literature), as justification for suspending, reducing or changing the medication. A change to an extended-release injectable was proposed, but the family did not have the resources to purchase the medication. He remained stable at the above dosage for about 12 months.
Due to the lack of judgement of illness and the reduction of family control due to the improvement in the following months, the patient neglected to take the AP, which became irregular until the treatment was completely abandoned. The family, perceiving behavioural changes similar to those that had caused his first hospitalisation, took him to the Institute for psychiatric consultation, where the patient admitted having abandoned the medication, arguing that he had gained weight and that he felt well.
On this occasion, another AP was started, aripiprazole 7.5 mg, but the patient did not attend his check-ups for the following six months; the abandonment of the medication was confirmed in the second hospitalisation ordered when the patient went to the emergency department in the same conditions as the first admission, equally agitated, distrustful, accusing his wife of infidelity; he was also brought against his will and with the support of the police. He was also brought in against his will and with the support of the police. The AP aripiprazole was prescribed during his hospitalisation, at a dose of 15 mg/day, with good tolerance and improvement of his symptoms. He was discharged from hospital after a little over two months of hospitalisation, at a dose of 30 mg/day, with the recommendations to maintain the treatment and to attend regular check-ups.
Discussion
Initially, it must be taken into account that patients with TD do not come to hospital spontaneously, but are generally forced to do so by the family or the legal authorities, because they firmly believe in the content of their delusional idea, which is the basic element for the suspicion of TD,1,10 as in the case presented. The patient firmly believes in the idea they hold and the content is completely possible within the socio-cultural context in which they live, making it a challenge for the clinician to discern whether the patient’s interpretation constitutes a real fact or not, so it is essential to corroborate with family members to ensure that the belief is not shared by others, as occurs, for example, in the religious context of some populations2. On the other hand, information from the family must be analysed meticulously to avoid legal problems later on,
since mental illness, due to the limitations of diagnostic tests, has been, on more than one occasion throughout history, a way to invalidate an individual or exclude him socially and legally since mental illness, due to the limitations of diagnostic tests, has been, on more than one occasion throughout history, a way to invalidate and exclude socially and legally an individual. One characteristic to take into account is that, during their discourse, patients tend to contradict themselves and to sustain their arguments on the basis of evidence that is not real and is the product of an interpretation that responds to their delusional construct14
Once it is established that the ideas are delusional, that they are not part of reality, it is necessary to rule out that they are not physiological effects of psychoactive substances or medication. To do this, it is necessary to list all the substances that the patient is consuming, from products considered “natural”, such as herbal teas, herbs, etc., to drugs or toxic substances15. The patient in the clinical case has a history of “acullico”, a process in which the alkaloids from the coca leaf are released into the saliva and absorbed by the mucosa; The indigenous Andean population has been doing this practice since time immemorial in order to obtain certain effects such as relief from thirst, hunger, sleep and physical fatigue, as well as being used in a medicinal, magical-religious, divinatory, symbolic and social way; currently this practice has spread to urban areas as a way of reaffirming its origins16,17,18. Studies on the possibility of coca leaf and its psychotic effects have ruled out this possibility, because it is estimated that for every gram of coca leaf, between 5 and 7 mg of cocaine is obtained, the same as that found in a bag of mate tea, which is legally marketed in Bolivia and Peru;17the levels of absorption and concentration of these alkaloids in the blood are highly variable and depend on many factors such as the species of the plant, the quantity of coca leaves or the alkali used in the process of acullico, as well as the consumer’s expertise in this practice16,17,19. Coca leaf alkaloids are related to psychotic manifestations, but this depends on the amount consumed, route of administration, individual predisposition, variety of the plant, among other factors; the amount of alkaloids absorbed from coca leaf through acullico is far from the values found in people who consume cocaine (as sulphate); 0.5-0.7% for the leaf, compared to 90% for the processed substance in powder form17. In users of cocaine in its various forms, psychotic manifestations are very frequent16. The patient had a sporadic habit of smoking coca leaf, something that intensified in order to stay awake and alert, due to the ideas in his head related to his wife’s infidelity; the consumption prior to the delirious ideas is not constant, so, due to the aforementioned characteristics of traditional coca leaf consumption, the origin of the delirious ideas cannot be attributed, but the intensification of anxiety as a stimulant substance can be attributed19.
In relation to alcohol, alcoholic jealousy or alcoholic celopathy has been described in the literature as a typical manifestation of alcoholic patients; a condition that has been little investigated and there are few studies in this group with publications that present important methodological flaws; according to Jimenez-Ariero (2007)20 this characteristic presented by alcoholic patients is considered an expression of fear and overvalued ideas with complexes associated with an intense emotional charge, without a delirious content per se, these people unconsciously recognise that they have failed in their role as husband and partner. In the clinical case presented, the patient was an episodic consumer of alcoholic beverages and, although there was an increase in consumption in the last period, he did not meet the criteria for alcohol abuse or alcohol dependence, this prior diagnosis being necessary to consider chronic alcoholic delirium21.
On the other hand, general medical conditions can manifest with alterations in mental state and the list is long, as can be seen in table 4, and the clinician must be aware of these possibilities in order to carry out a thorough anamnesis and physical examination and then, depending on the suspicions, request complementary studies to confirm or rule out the suspected pathologies. It is essential to rule out all the possibilities before stating that it is a TD1-3,11,21. In particular, mention is made of acute confusional syndrome (delirium), which is an expression of an organic pathology that, in addition to delusional ideas, causes impairment of attention, language, executive functions, among other areas, and it is this set of characteristics that lead us to rule out TD2,15. Neurocognitive disorders also manifest with alterations in several cognitive areas and arise in older patients. Both conditions were ruled out in the patient as cognitive functions were preserved; from admission the patient was globally oriented, euproséxico, with preserved memory, coherent, organised and relevant speech and intelligence within the normal range. It is essential to consider these pathologies for the differential diagnosis, because the course and prognosis, with timely and appropriate treatment, is completely different from TD, all the symptoms remit completely, without being a psychiatric disorder per se. This requires a detailed anamnesis, a thorough physical examination and a thorough mental status examination1,2,21.
With regard to psychiatric pathologies, the differential diagnosis should be made especially with mood disorders, bipolar disorder or depression, schizophrenia and brief psychotic episodes1,2,15.
To think of a mood disorder, such as bipolar disorder, delusions should appear in the context of an elevated mood, which becomes expansive and/or irritable, accompanied by increased energy and in a cyclical or episodic manner1,2,15,21. The patient’s delusions are constant and no mood alterations are identified, with worsening in the last year without any cyclical oscillation, the picture remained constant over time. In the case of major depression with psychotic symptoms, in which, associated with the history of depressed mood, delusional ideas can be found; but in the patient, there was no history of depressed mood prior to the onset of the picture; there were moments of intense suffering, but related to the ideas of his wife’s infidelity associated with possible repercussions in marital and family life.
Schizophrenia is another pathology with which a differential diagnosis should be made due to shared characteristics such as chronicity, insidious progression, the presence of hallucinations and delusions. In schizophrenia, delusions are generally persecutory, scarce, episodic, bizarre, without social propagation (credibility of the environment) and do not constitute the central axis of the disorder, which is given by hallucinations; the patient has disorganised behaviour and there is an impairment of other spheres with a greater global compromise1,2,22. In TD, the central axis is delusional ideas, they are present continuously, they are well systematised and therefore have social propagation, patients maintain functionality in coherence with their delusional context and do not present cognitive impairment or destructuring of the self22.
Hallucinations may occur, but they are sporadic and related to the delusional content1-3,11,22. The patient has the firm idea that his wife is unfaithful, which is entirely possible, so it is not an absurd idea, on the other hand, the patient presents sporadic sensory-perceptual alterations related to the context of the delusional ideas, he presents a good level of functioning, although this has deteriorated in the last year, he is not disorganised as an individual.
It is essential to determine the seriousness and the need for intervention in the case of a person with delusional ideas; it is very difficult for a patient to come to the clinic spontaneously, to start pharmacological treatment voluntarily and on an outpatient basis; in general and as in the clinical case presented, patients come late, when the repercussions on the environment are important or involve risks.
After ruling out all the previously-mentioned differential diagnoses and establishing that the case corresponds to a celotypic type of TD, treatment should be started with a AP as the main medication, with the aim of achieving symptom remission. In about 60% of patients, symptomatology is reduced after 12 weeks of treatment, and one of the great challenges is to ensure that patients comply with the therapeutic guidelines, as they do not believe themselves to be ill 1,2,22,23.
Antipsychotics should be chosen according to the characteristics of the patient, seeking greater benefit versus adverse effects, and until the ideal drug dose is found, in most cases, many trials must be carried out1,2,2,23.
In this patient, risperidone was used and the dose was increased slowly and progressively until a balance was found between symptom control and side effects. Although the response to symptomatology was partial, increasing the dose was not an option, as the maximum dose established in the literature had been reached and increasing the dose would only cause more adverse effects. With partial control of the symptoms, the patient was able to return to his activities, but due to the abandonment of the medication, justified by the weight gain associated with the poor perception of illness, the patient was readmitted to the psychiatric center, with the same symptomatic picture described on his first admission, the central axis of which were the ideas of his wife’s infidelity. In the second admission, another antipsychotic medication, aripriprazole, was chosen, taking into account the patient’s visible weight gain. He was discharged from hospital after more than a month of hospitalisation, with the most intense symptoms under control and with recommendations to continue outpatient follow-up for psychotherapy and pharmacological control1,2,23.
The above-named patient has an unfavourable prognosis because the celotypic presentation subtype is more difficult to remit despite continuous treatment; he also has some personal characteristics that are related to a worse course, such as being male, insidious onset, late diagnosis, no triggering factor, lack of understanding of the disorder and partial response to the antipsychotic drugs used1,2,10. Furthermore, people suffering from TD in Bolivia face an additional difficulty, a reduced range of possibilities for PD and administration routes, associated with the absence of a public health system that guarantees mental health care to the population and the high costs of medication; all these factors together are responsible for people with TD being untreated and, in many cases, potentially dangerous for those around them, as in the case presented.
It is essential that the State changes its public health policies to provide mental health care for its population by allocating sufficient economic resources to enable the hiring of mental health professionals in the public health system and the subsidising of medication for severe mental disorders.
Ethical Responsibilities
The author declares that she has followed the established protocols on the publication of patient data, respecting confidentiality, having informed the patient and his/her relatives about the presentation of the case and obtained their written informed consent, a document that is in the possession of the author of the article.
Conflict of interest
The author declares that there is no conflict of interest.
Acknowledgements
Thanks to: the patient and family for consenting to the publication of the clinical case, the Instituto Psiquiátrico San Juan de Dios for allowing access to the patient’s clinical history data, and to Licenciada María Isabel Peñaloza Chej for proofreading
References
1. Palomo T, Jimenez-Ariero MA. Manual de Psiquiatria Madrid: Gráfica Marte; 2009.
2. Sadock B, Sadock V, Ruiz P. Compendio de psiquiatria, ciencia do comportamento e psiquiatria clinica. 11th ed. Porto Alegre: Artmed; 2017.
3. Organización Mundial de la Salud. Clasificacio4n Estadi4stica Internacional de Enfermedades y Problemas Relacionados con la Salud - CIE 10 Wahsington: OMS; 2008. [ Links ]
4. Román AN, Esteve DN, Donomarco ML , Domínguez FC, Portugal E, Rivero F. Diferencias de genero en el trastorno delirante. Rev. Asoc. Esp. Neuropsiq. 2015 ene/mar; 35(125).
5. Gonzalez-Rodriguez et al. Trastorno delirante: no hay diferencias de genero en las edades de inicio, ideación suicida o comportamiento suicida. Rev. Brasileña de Psiquiatria. 2014; 36(2).
6. Mármol BF, Luque LR, Farouk AM, Fernandez-Creuhet NR. Estudio descriptivo de series de casos de tratorno delirante. Rev Chilena de Neuropsiq. 2015; 53(4). [ Links ]
7. Díez PA. Psicopatologia de la interpertación delirante. Rev de la Asoc Esp de Nueropsiq. 2003 sep;(87). [ Links ]
8. Olivo AP. La mente delirante. Psicopatologi4a del delirio. Revista Chilena de Neuropsiquiatri4a. 2009; 47(1).
9. Gonzalez-Rodriguez A, et al. Estudio retrospectivo del tratamiento y uso de consultas en un grupo clínico de pacientes con trastorno delirante. Rev Salud Mental y Psiquiatria. 2014 abr/jun; 7(2). [ Links ]
10. Salavert J, Berrospi M, Miralles RM, Dueñas ML, Tiffon L. El tratorno delirante. Revisando aspectos de la paranoia. Rev Psiq Fac Med Barna. 2003; 30(6). [ Links ]
11. American Psychiatric Association. Guia de consulta de los criterios diagnósticos del DSM-5 Londres y Washington: APA; 2014. [ Links ]
12. Baldaçara L, Fiorani BJ. Tratamento do trastorno delirante persistente. Arq Med Hosp Fac Cienc Med Santa Casa de Sao Paulo. 2009; 54(2).
13. Shelton M, Ahmad KW, Thacker SP. Biblioteca Cocchrane. [Online].; 2015 [cited 2020 enero 15. Available from: https://www.cochranelibrary.com/es/cdsr/doi/10.1002/14651858.CD009785.pub2/full/es.
14. Mármol BF, Luque LR, Farouk AM, Fernandez-Creuhet NR. Tratorno delirante y conducta suicida: estudio descriptivo. Rev. Chilena de Neuropsiq. 2018; 56(4). [ Links ]
15. First MB. DSM-5 Manual de diagnóstico diferencial. 1st ed. Association AP, editor. Madrid: Panamericana; 2015.
16. Instituto Boliviano de Altura. Uso de la hoja de coca y salud pública. 1st ed. Villena C M SM, editor. La Paz; 1997.
17. Díaz A. Hoja, pasta, polvo y roca. El consumo de los derivados de la coca. Barcelona UAd, editor. Barcelona: Publicacions d’Antropologia Cultural; 1998.
18. DDHH. ELEMENTA. Revision sistematica de articulos cientificos de uso medicinal, tradicional y agroindustrial de la hoja de coca y sus derivados. 1st ed. Colombia: Khoka Alternativa; 2018.
19. Vera ZK, Menrique VG. Aspectos farmacologicos y socioculturales del consumo de hoja de coca en indígenas koguis respecto al consumo d ecocaina en ambientes urbanos. Rev Internacional de Psicologia. 2002 julio; 3(2).
20. Jime4nez-Arriero MA, Herna4ndez B, Mearin MI, Rodri4guez-Jime4nez R, Jime4nez GM, Ponce AG. Celopati4a alcoho4lica: un antiguo y actual dilema. Rev Adicciones. 2007; 19(3). [ Links ]
21. Henry E, Bernard P, Brisset C. Tratado de psiquiatria. 8th ed. Masson , editor. Barcelona; 1978.
22. Díaz D, Mancilla F, Ortiz C, Osorio A. Trastorno delirante. Caso de una reunión clínica. Rev Psiq y Salud Mental. 2017; XXXIV(3/4). [ Links ]
23. Jufe G. Psicofarmacología practica. 3rd ed. Buenos Aires: Polemos; 2012.
24. Medicos Internos Residentes (MIR). Manual del residente de psiquiatria Madrid: Marte; 2012. [ Links ]

