Introduction
According to the American Speech,
Language and Hearing Association (ASHA), a communication disorder “is an
impairment in the ability to receive, send, process, and comprehend concepts or
verbal, nonverbal and graphic symbol systems” [1].
Therefore, in general terms, a communication disorder may be represented as a hearing
loss (receive), language disorder (receive, send, process and/or comprehend),
and/or speech production disorder (send). Voice disorders are a common
work-related health problem
among teachers, with a prevalence up to 80% of all reported voice disorders in
a year [2]. According to the Organization
for Economic Cooperation and Development (OECD, an intergovernmental economic
organization consisting of 35 member countries), some of the primary factors
that affect the working lives of teachers include teaching hours, the extent of
non-teaching duties, salaries, and average class size [3].
Further detailed in the report, approximately 35% of teachers were at least 50
years of age in 2013, and more than 67% of teachers were women. Therefore, the
analysis of the health and aging process in this occupational group should consider
both work-related and individual factors in order to identify those conditions
that influence teachers’ health [4].
Voice disorders among teachers are multifactorial
conditions.
For example, previous research demonstrated that French teachers with voice
disorders had higher levels of psychological distress, including an 80% greater
risk of a major depressive episode and 70% for general anxiety disorder [5]. A recent systematic review of literature
reported a statistically significant association between the increased
occurrence of voice disorders among teachers with high stress at work and less
than 6 hours/day of sleep [6]. These
findings suggest a comorbidity between voice and psychological disorders and
support recommendations of including techniques for stress levels reduction
among occupational voice users [7]. Another
important but not well-explored health problem among teachers is hearing loss: previous
research involving Brazilian and Swedish teachers reported a prevalence of hearing
loss and tinnitus among teachers of 25% [8] and
31% [9], respectively.
A lowering of the quality of life among teachers has
been associated with work-related health problems like voice disorders and
stress [10,11]. Nevertheless, there is a
dearth of studies on how such health conditions influence employment retention
and disability. This
is partially due to the fact that few large country wide databases, which
contain this type of data, exist. One such database is used by the Colombia’s National
Board of Disability Assessment (NBDA). This database was created for the
collection, processing, and retrieval of the data on occupational diseases,
with the main purpose of properly recording country-wide data from each
ascertained case. This database includes information on sociodemographic
characteristics, type and nature of disease, and percentage of impairment, disability,
or handicap. Further, specific guidelines are outlined to perform assessments
and define the nature of the disease and magnitude of the disability.
The
Colombian NBDA database provides a useful tool to conduct a retrospective study,
examining the influence of various health conditions on employment retention
and disability. The current study proposes the following three aims: 1. define the
occurrence of work-related hearing problems and voice disorders among teachers
that have contacted the Colombian NBDA for follow-up; 2. identify individual
associated factors of hearing problems and voice disorders among teachers; 3. assess
the limitations and restrictions (in
terms of disability and handicap) due to hearing problems and voice
disorders among these participants. With such information, researchers and
health care providers will be able to better focus on factors hampering teachers’
ability to teach effectively.
Methods
This retrospective study consists of a review of the
National Database (2007-2014) of the Colombian National Board of Disability
Assessment (NBDA). The NBDA contains information related to all various diseases
and disabilities (occupational and non-occupational cases). The second author
obtained permissions to use this database for the current analysis.
NBDA definitions and
protocols
The NBDA database was created for
the collection, processing, and retrieval of the data on occupational diseases,
with the main purpose of properly recording country-wide data from each case.
This database includes information on sociodemographic characteristics, type
and nature of disease, and percentage of impairment, disability, or handicap. The
definition of these three terms was adopted from the International Classification of Impairments, Disabilities and Handicaps,
published by the World Health Organization (WHO) in 1980, with the following
distinctions: impairment is defined as any loss or abnormality of
psychological, physiological or anatomical structure or function; disability, as any restriction or lack of
ability to perform an activity in the manner or within the range considered
normal for a human being; and handicap, as an impairment which prevents an individual from fulfilling
a normal life role [12].
The percentage of each (impairment,
disability, handicap) was calculated based on the legislation of
the Colombian Minister of Work [13]: the
percentage of impairment range from 0 to 50; disability, from 0 to 20; and handicap´s,
from 0 to 30. The sum of the three items is the total work capacity loss.
According to Colombian regulations, the pension for disability is given if the
total sum exceeds 50% of total work capacity loss.
When a worker is injured or gets
sick, he/she goes to a physician who determines if the issue is work-related,
which means that it must be: 1. associated with a health hazard present in the
work environment and 2. included in the Colombian list of occupational diseases
Decree 1477 of 2014 [14].
If the worker does not agree with the conclusion of the physician, she/he
receives a third-part assessment by one of four NBDA commissions, which consist
of four professionals in charge of the evaluation and classification of the
cases: two occupational physicians, one therapist or psychologist and one
lawyer with specialization in health issues. Until February of 2015, the NBDA
used Law 917 of 1999, which adopted the definitions of the International
Classification of Impairments, Disabilities and Handicaps [12],
as a guideline to perform their assessments and define the nature of the
disease and magnitude of the disability.
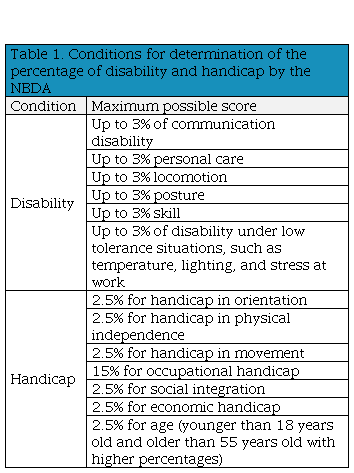
For the determination of the
percentage of impairment, disability and handicap related to voice and hearing
problems, the NBDA uses instruments and protocols determined by speech and
language pathologists and audiologists. Table 1
shows the conditions for determination of the percentage of disability and
handicap by the NBDA.
Table 1
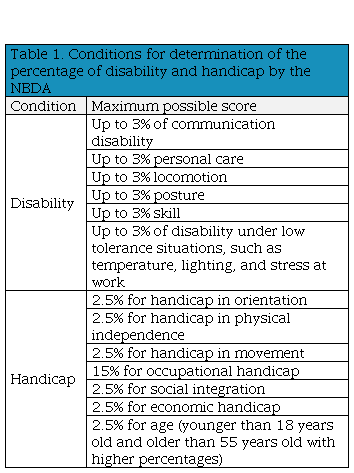
| Conditions for determination of the percentage of disability and
handicap by the NBDA
|
|
Condition
|
Maximum possible score
|
|
Disability
|
Up
to 3% of communication disability
|
|
Up
to 3% personal care
|
|
Up
to 3% locomotion
|
|
Up
to 3% posture
|
|
Up
to 3% skill
|
|
Up
to 3% of disability under low tolerance situations, such as temperature,
lighting, and stress at work
|
|
Handicap
|
2.5%
for handicap in orientation
|
|
2.5%
for handicap in physical independence
|
|
2.5%
for handicap in movement
|
|
15%
for occupational handicap
|
|
2.5%
for social integration
|
|
2.5%
for economic handicap
|
|
2.5%
for age (younger than 18 years old and older than 55 years old with higher
percentages)
|
Therefore, from the percentage’s
distribution, the focus of the evaluation of disability is on health conditions
and mobility restrictions, whereas for handicap is on occupation and mobility.
General information
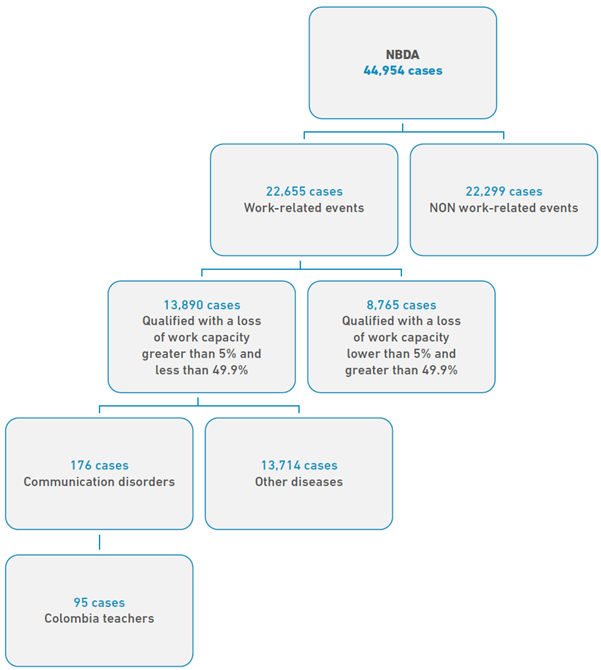
From 2007 to 2014, the NBDA
received 78,920 claims, corresponding to 44,954 people of all around the
country. Among the procedures sent to the NBDA, 22,655 cases (around 50%) were identified
as work-related events (work accident or occupational disease). A
case was “defined” as work related if the disease was identified as a
consequence of the worker’s working conditions. In order to define this, the
members of the NBDA request evaluations and reports of the physical and
environmental conditions to which the worker was exposed. Additionally, the
worker provides his/her medical history. With this information, the members of
the NBDA evaluate the association between either the accident or the disease
with the working conditions to determine the work-relatedness of the event.
As shown in Figure 1, among the work-related identified events, 13,890
people were qualified with a loss of work capacity between 5% and 49.9%. This
means that approximately 60% of the claims were qualified with a partial
permanent disability (they had limitations to their ability to continue
performing their jobs as they did before the accident or disease). The
quantification of the loss of work capacity was made based on Decree 917 of
1999, which defines the criteria for determination of the percentage of
impairment, disability, and handicap [15].
According to the Article 8 of this Decree, total percentage of work capacity
loss is defined using three aspects: impairment (0% to 50%), disability (0% to 20%),
and handicap (0% to 30%). This Colombian Decree is based on the Guides to the Evaluation of Permanent Impairment,
published by the American Medical Association [16].
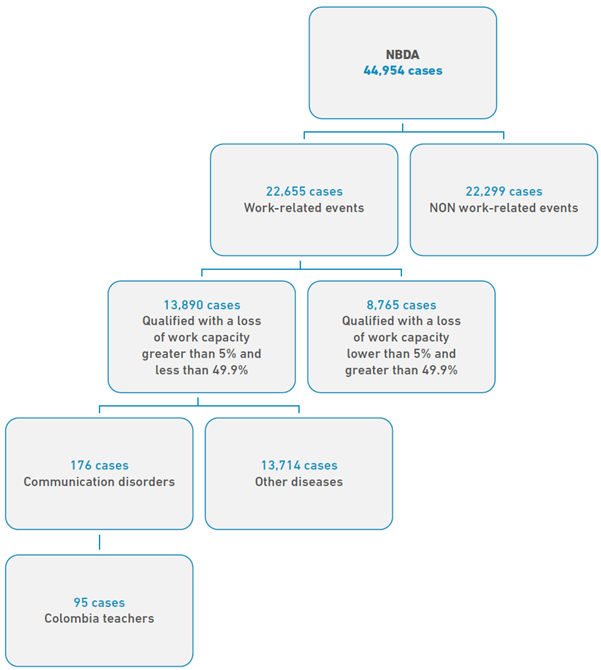 Figure 1
Flowchart of NBDA search and selection of Colombian teachers with communication
disorders
Figure 1
Flowchart of NBDA search and selection of Colombian teachers with communication
disorders
The
database used for this study contains information on individual factors, such
as occupation, gender, age, level of education, marital status, city, clinical diagnosis
code (according to ICD-10), percentage of impairment, percentage of disability,
and percentage of handicap.
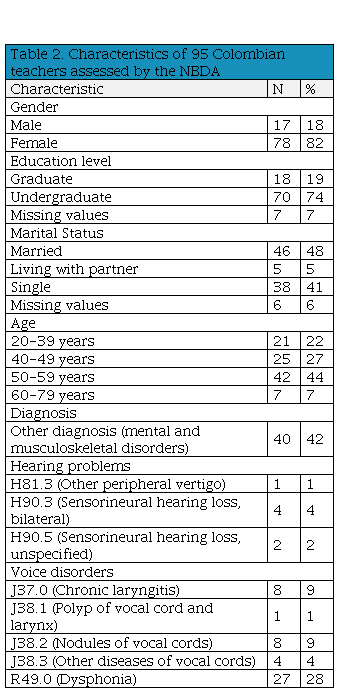
Participants
The
review of the database identified 95 Colombian teachers who had contacted the
NBDA for follow-up and were listed in the NBDA between 2007 and 2014. Of those,
teachers with communication disorders were identified (n=95).
As
shown in Table 2, the clinical diagnosis
codes considered for the current study to be related to hearing problems and
voice disorders were: J37.0 (Chronic laryngitis), J38.1
(Polyp of vocal cord and larynx), J38.2 (Nodules of vocal cords), J38.3 (Other
diseases of vocal cords), R49.0 (Dysphonia), H81.3 (Other peripheral vertigo),
H90.3 (Sensorineural hearing loss, bilateral), and H90.5 (Sensorineural hearing
loss, unspecified).
Table 2
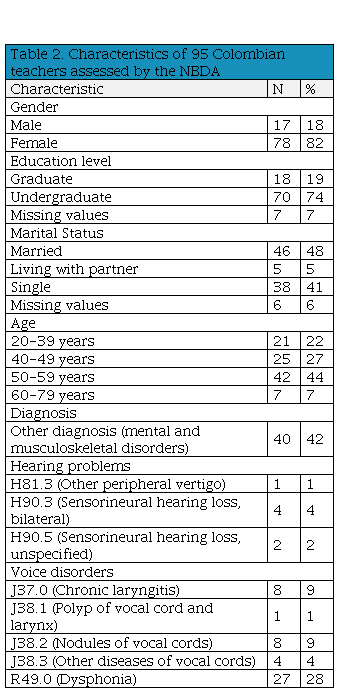
| Characteristics
of 95 Colombian teachers assessed by the NBDA
|
|
Characteristic
|
N
|
%
|
|
Gender
|
|
Male
|
17
|
18
|
|
Female
|
78
|
82
|
|
Education
level
|
|
Graduate
|
18
|
19
|
|
Undergraduate
|
70
|
74
|
|
Missing
values
|
7
|
7
|
|
Marital
Status
|
|
Married
|
46
|
48
|
|
Living
with partner
|
5
|
5
|
|
Single
|
38
|
41
|
|
Missing
values
|
6
|
6
|
|
Age
|
|
20-39
years
|
21
|
22
|
|
40-49
years
|
25
|
27
|
|
50-59
years
|
42
|
44
|
|
60-79
years
|
7
|
7
|
|
Diagnosis
|
|
Other
diagnosis (mental and musculoskeletal disorders)
|
40
|
42
|
|
Hearing
problems
|
|
H81.3
(Other peripheral vertigo)
|
1
|
1
|
|
H90.3 (Sensorineural
hearing loss, bilateral)
|
4
|
4
|
|
H90.5
(Sensorineural hearing loss, unspecified)
|
2
|
2
|
|
Voice disorders
|
|
J37.0
(Chronic laryngitis)
|
8
|
9
|
|
J38.1
(Polyp of vocal cord and larynx)
|
1
|
1
|
|
J38.2
(Nodules of vocal cords)
|
8
|
9
|
|
J38.3
(Other diseases of vocal cords)
|
4
|
4
|
|
R49.0
(Dysphonia)
|
27
|
28
|
Definitions of voice disorders and hearing
problems in the NBDA database
The
NBDA gives specific procedures for the identification and classification of
health conditions, including of voice disorders and hearing problems.
Voice
disorders
As part of the required examinations to define a voice disorder, an ENT specialist performed a clinical exam, including a laryngoscopy. After the examinations, the NBDA analyzed the results, which included a diagnosis code (ICD-10). For voice disorders, the clinical diagnosis codes considered, according to ICD-10, were listed in Table 2. After receiving information related to the working conditions and the medical history, the members of the NBDA determined the level of impairment. This level was determined by considering three questions: 1. how well could the teacher make himself/herself be heard? 2. how intelligible was the teacher? and 3. how efficient was the speech of the teacher? The percentage of impairment was determined based on Table 13.8, Impairment related with speech problems, in the Decree 917 of 1999 [15].
Hearing problems
Teachers went through a complete hearing assessment (bone and air conduction audiometry + speech audiometry + impedance audiometry) at least three times for 1-2 months. Considering the Decree 917 of 1999, the hearing threshold level, using audiometry, was defined based on the pure tone average at frequencies of 0.5, 1, 2, and 4 kHz. Binaural impairment was determined by means of the following formula [15]:
Binaural hearing impairment (%) = (5 x % hearing impairment better ear) + (% hearing impairment poorer ear) x 0.5
The percentage of
hearing impairment was determined based on Table 13.7, Binaural Hearing
Impairment, in the Decree 917 of 1999 [15].
Statistical
Analysis
Using the information
from the 95 teachers found in the NBDA, data on individual factors (gender,
age, level of education, marital status), diagnosis code, and percentage of
work capacity lost were extracted from the NBDA database and analyzed using SPSS
22 software. Descriptive statistics were used for characteristics of the study
population. The Shapiro-Wilk test was used to evaluate whether variables were
normally distributed. To assess the association between
individual characteristics and work-related hearing problems and voice
disorders among teachers, a multiple logistic regression analysis was used. Variables
with a p-value below 0.20 in the univariate analyses were included in the
multivariate analysis in order to avoid residual confounding [17], and were only retained when the p-value
reached the conventional level of significance of 0.05. The magnitude of the
association was expressed by the odds ratio (OR), and the statistical
significance as the 95% confidence interval (95% CI).
Results
In
total, epidemiological records from 95 teachers with communication disorders were
available in the NBDA database; all were used for this study. Of these 95
teachers, most were females (82%), and most were between 50-59 years of age (44%).
Table 1 shows that 51% of the teachers were
identified with voice disorders, whereas 7% were identified with hearing
problems.
Individual
factors associated with hearing problems and voice disorders among teachers
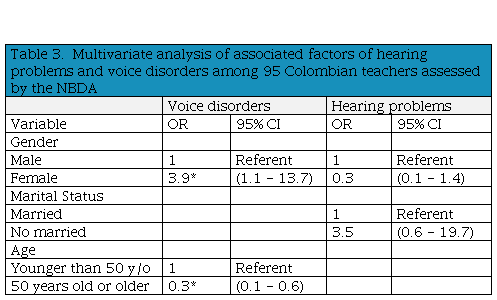
Table 3 shows the associated
factors of hearing problems and voice disorders among the 95 teachers. In the univariate
analysis, gender was significantly associated with voice disorders and hearing
problems. Nevertheless, after adjustments for
significant factors in the univariate analysis (marital status and age), the
association between gender with hearing problems did not remain significant.
Multivariate analysis shows that participating female teachers were 4 times
more likely to be identified with voice disorders compared with their male
colleagues. The results of the multivariate analysis also show that teachers 50 years old or older were less likely (OR= 0.3)
to be identified with voice disorders by the NBDA than younger teachers.
Table 3
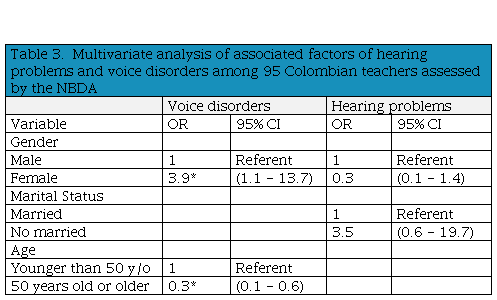 *
p<0.05
*
p<0.05
| Multivariate analysis of associated factors
of hearing problems and voice disorders among 95 Colombian teachers assessed
by the NBDA
|
|
Voice disorders
|
Hearing problems
|
|
Variable
|
OR
|
95% CI
|
OR
|
95% CI
|
|
Gender
| | | | |
|
Male
|
1
|
Referent
|
1
|
Referent
|
|
Female
|
3.9*
|
(1.1 - 13.7)
|
0.3
|
(0.1 - 1.4)
|
|
Marital
Status
| | | | |
|
Married
| | |
1
|
Referent
|
|
No
married
| | |
3.5
|
(0.6 - 19.7)
|
|
Age
| | | | |
|
Younger
than 50 y/o
|
1
|
Referent
| | |
|
50
years old or older
|
0.3*
|
(0.1 - 0.6)
| | |
Impairment,
disability, and handicap among teachers
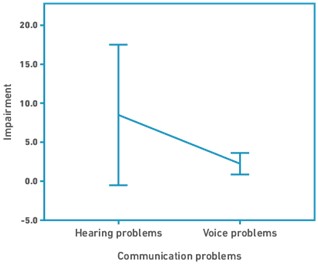
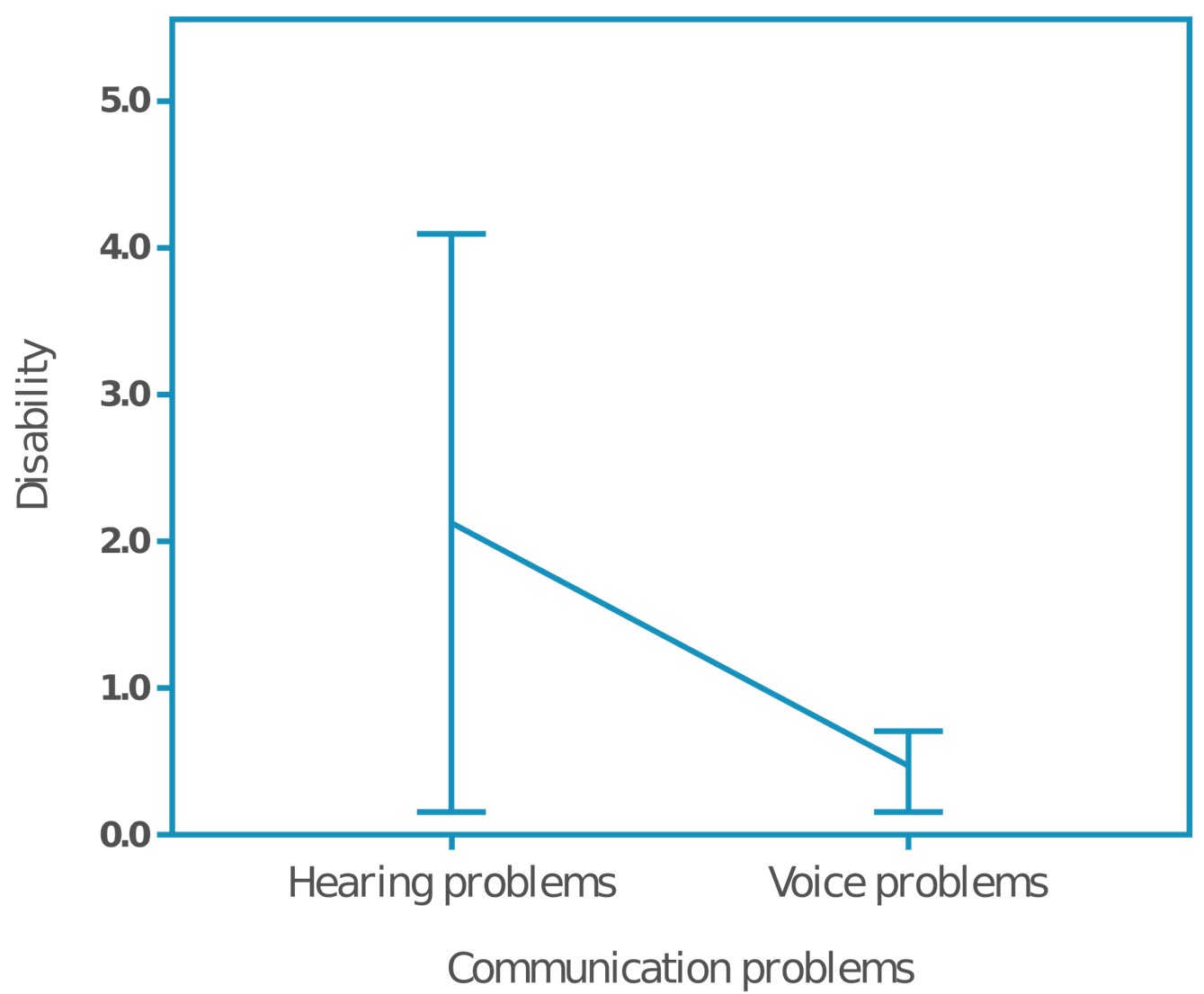
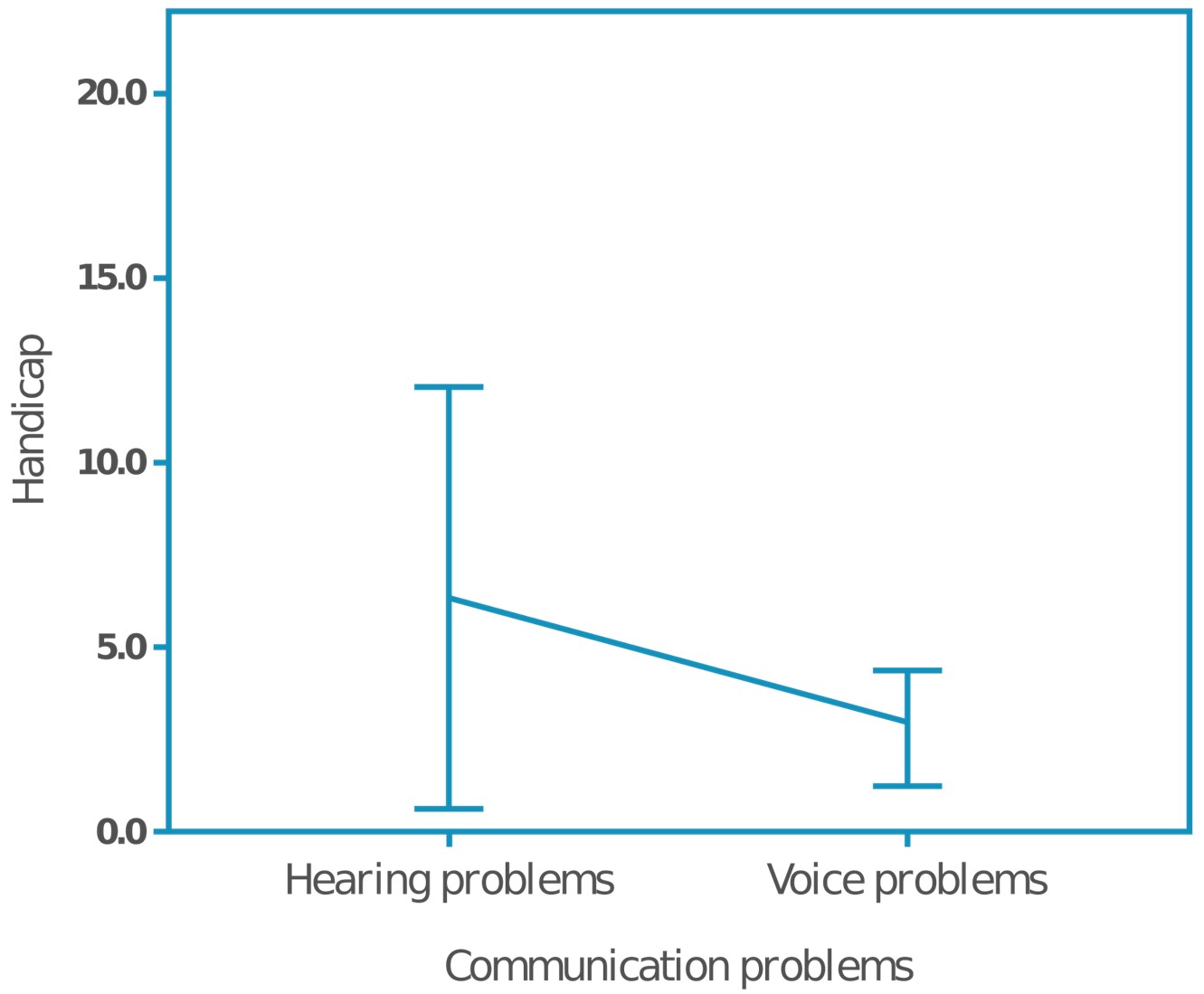
Among
the 95 Colombian teachers with hearing problems and voice disorders, the occurrence
of hearing problems was lower than voice disorders. However, the members of the
Colombian NBDA considered that hearing problems caused higher impairment,
disability and handicap compared with voice disorders (impairment= 9% vs. 2%,
disability= 2% vs. 1%, and handicap= 6% vs. 3%). Figure
2.a shows the mean values and standard error of impairment by hearing
problems and voice disorders. Figure 2.b and
Figure 2.c show that voice disorders,
although more prevalent among included teachers, were defined by the NBDA with lower
disability and handicap values (respectively).
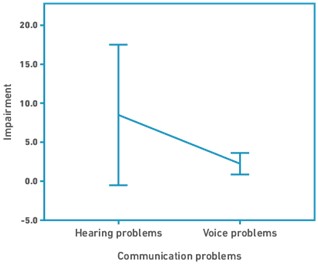 (a)
Mean percentage of impairment score per communication disorder
(a)
Mean percentage of impairment score per communication disorder
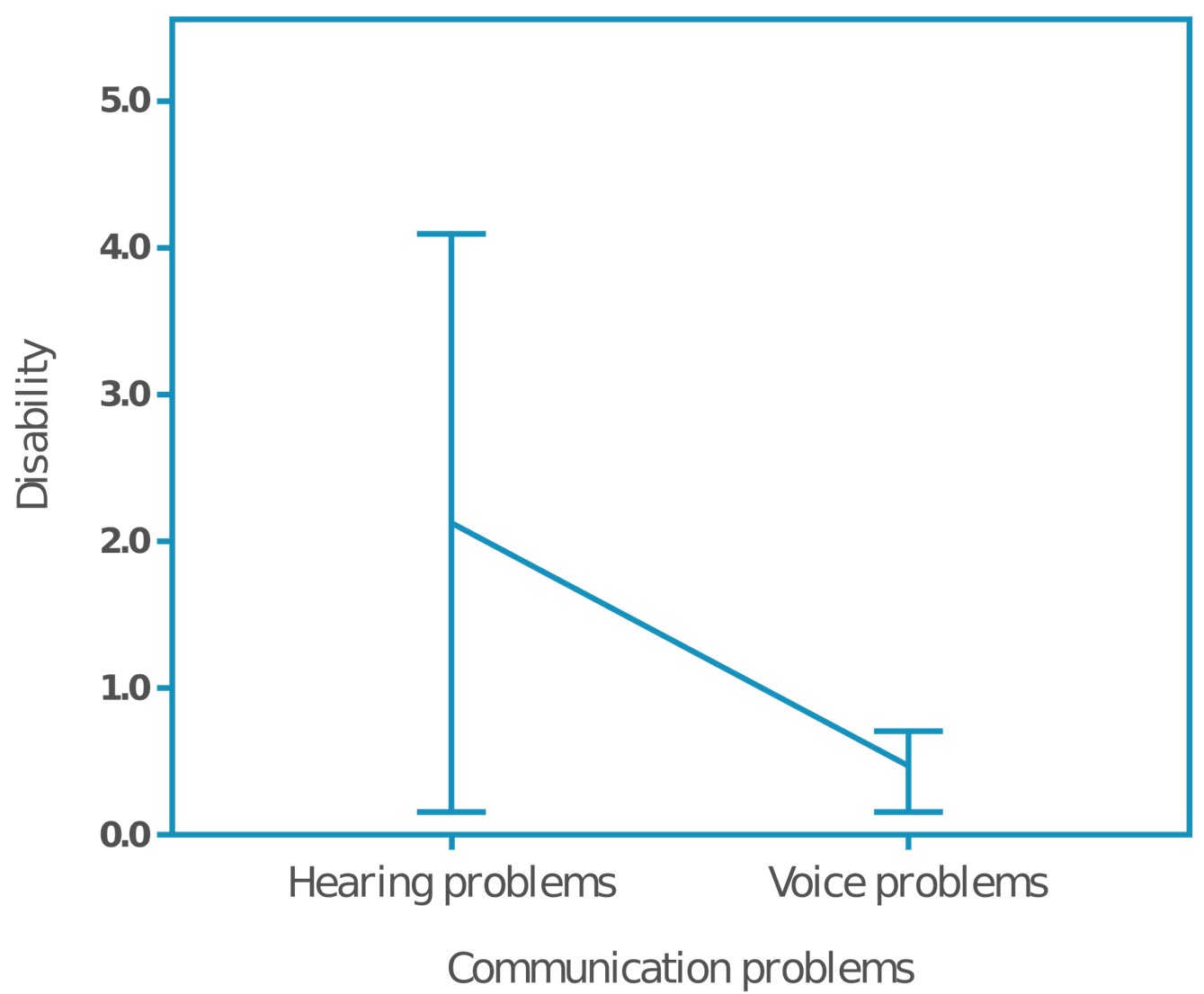 (b)
Mean percentage of disability score per communication disorder
(b)
Mean percentage of disability score per communication disorder
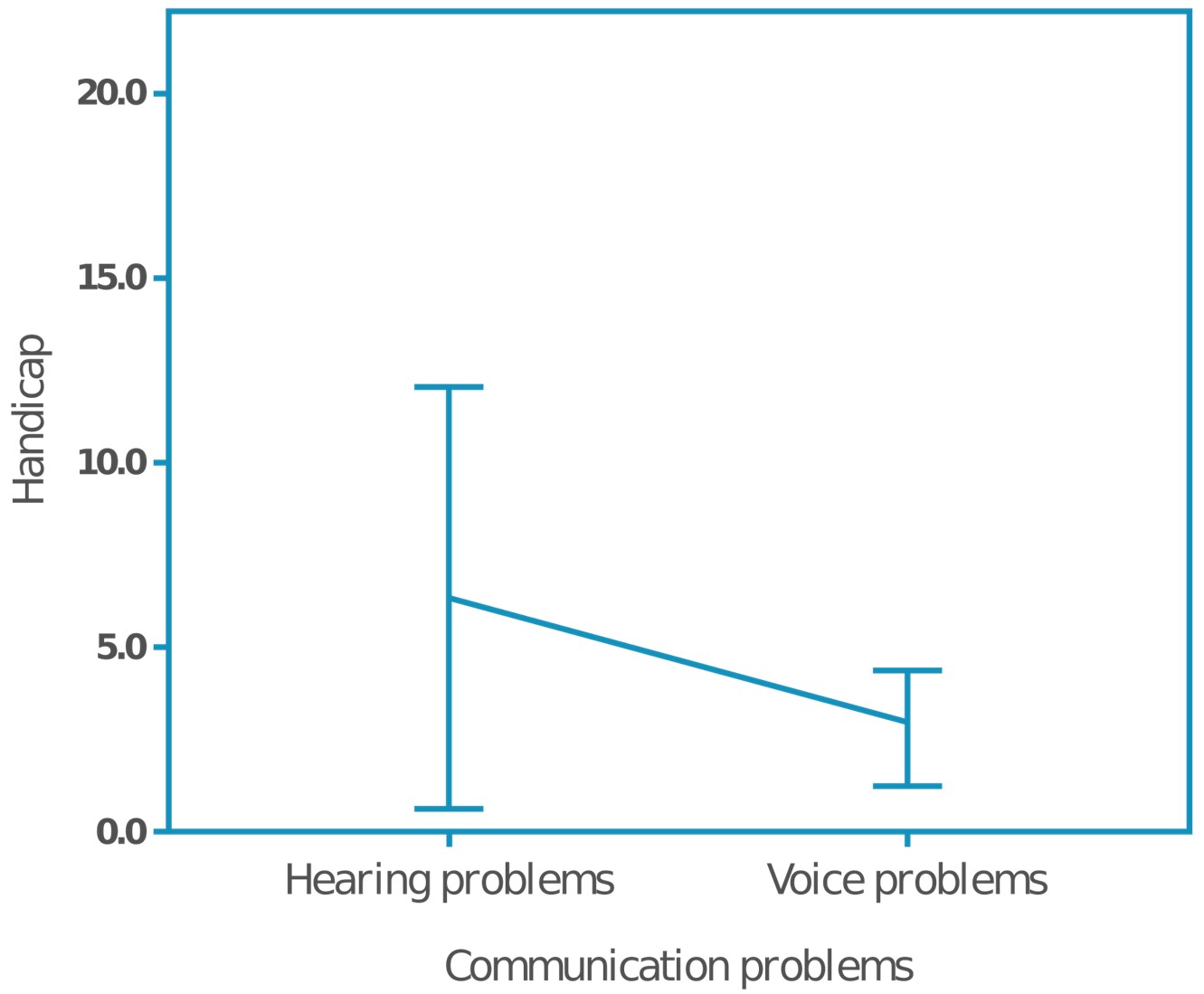 (c)
Mean percentage of handicap score per communication disorder
Figure 2. Mean percentage score among 55 Colombian teachers identified with communication disorders
by the NBDA: (a) mean percentage of impairment score per communication
disorder, (b) mean percentage of disability score per communication disorder,
(c) mean percentage of handicap score per communication disorder.
(c)
Mean percentage of handicap score per communication disorder
Figure 2. Mean percentage score among 55 Colombian teachers identified with communication disorders
by the NBDA: (a) mean percentage of impairment score per communication
disorder, (b) mean percentage of disability score per communication disorder,
(c) mean percentage of handicap score per communication disorder.
Discussion
This
retrospective study of teachers that have contacted the Colombian National
Board of Disability Assessment (NBDA) for follow-up aimed to determine the
impairment, disability, and handicap associated with hearing problems and voice
disorders among Colombian teachers, as well as to assess the individual
associated factors. Results are dependent on the NBDA criteria and protocols.
Based on the data within those criteria and protocols, our results indicated
that although voice disorders were more prevalent than hearing problems, since hearing
problems can also affect the social integration in addition to the occupational
handicap, they were identified with higher impact upon the teachers by the
members of the Colombian NBDA.
In this study, around 51% of Colombian teachers were identified
as having a work-related voice disorder. Although our participants were
teachers that have contacted the Colombian NBDA for follow-up, our results are
in line with previous studies that reported a point prevalence of 45% among
Colombian teachers [18], and 57% among
Spanish teachers [19].
It has been reported that teachers have higher likelihood of having voice
disorders compared with other occupations, due in part to high vocal demands,
poor acoustic conditions inside the classrooms, and lack of vocal training [2, 20-22]. Cantor and Burdorf (2016) suggested
that voice disorders are persistent health problems among teachers, which is
reflected in a high prevalence, incidence and chronicity during one year
follow-up [23]. This high persistence of
voice problems among teachers may be partially explained because voice
disorders as a health problem among teachers are not identified as a health
problems by them, which means that teachers with voice complaints continue
working as much as possible despite their voice symptoms [24,25], thereby aggravating them. From our
results, it seems that physicians do not identify work-related voice disorders
easily either, considering 51% of the teachers looking for follow-up were
identified with a work-related voice disorder, whereas 7% of them were
identified with a work-related hearing problem.
Concerning
the individual factors associated with voice disorders, our results suggested
that female teachers in Colombia that have contacted the Colombian NBDA for
follow-up were more likely to have work-related voice disorders compared with
male teachers (OR= 3.9), whereas teachers 50 years old or older were less
likely to present work-related voice disorders compared with younger teachers
(OR= 0.3). These findings are in line with previous studies that report that
females (teachers and non-teachers) have a higher prevalence of voice disorders
generally [26] and that female teachers are
particularly at risk of being referred to vocal health professionals [27]. This voice-gender disparity may stem from
gender differences related to both laryngeal and non-laryngeal physiology, as
well as the effects of hormones and behavior [28].
As for the age effect, there are two possible explanations. First, it is likely
that more experienced teachers are easily identified with a work-related voice
disorder during the first examination of the physician. Second, more
experienced teachers are accustomed to experiencing occupationally related
vocal fatigue or voice problems and because they consider it normal, are less
likely to pursue disability claims.
In this study, of the 95 teachers that have contacted the
Colombian NBDA for follow-up, we found 7% with work-related hearing problems.
This finding is lower than the Brazilian study of Garcia Martins et al. (2007)
and the Swedish study of Sjödin et al. (2012), which found a prevalence of hearing
loss of 25% [8] and 46% [9], respectively. One possible explanation for
the decreased prevalence reported in our study is our population
characteristics. From our results, it seems likely that physicians doing the
first examination were better at detecting and accepting work-related hearing
problems than work-related voice disorders. Therefore, a small percentage of
teachers with hearing problems contacted the Colombian NBDA for follow-up. This
finding may be an indication that physicians identified easier hearing problems
than voice disorders as work-related health problems, even though both
communication processes impact quality of work and quality of life among
teachers. Another explanation may be related with the type of assessment
process implemented for the definition of hearing loss. In the present study,
teachers were required to undergo a complete hearing assessment (which included
not only a bone and air conduction audiometry, but also speech audiometry and impedance
audiometry) at least three times for 1-2 months. In Colombia, the repeated
measurements are used to assess the occurrence of a persistent hearing problem
and to diagnose the type and severity of hearing loss (also the
work-relatedness). In contrast, Garcia Martins et al. reported that
participants underwent pure tone audiometry and speech audiometry (once),
whereas Sjödin et al. used self-reports about the subjective hearing status;
therefore, these reduced requirements would likely show a higher prevalence of hearing
loss due to the type of evaluation implemented. This finding aligns with
previous voice disorder studies, which found an overestimation of teachers’ self-reported
voice disorders compared with perceptual identification by speech-language
pathologists [2]. A third possible
explanation may be the thresholds defined in the studies. In the Brazilian
study, hearing loss was defined as a 25dB reduction of the audiometric
threshold at 4,000 and 6,000Hz only [8]. In
the Swedish study, hearing loss was defined as a mean threshold larger than 35
dB HL for the frequencies 2000 Hz and 3000 Hz, and a mean threshold larger than
45dBHL for the frequencies 4000 Hz and 6000 [9].
The Brazilian and Swedish studies used just high frequencies to define hearing
loss, whereas the NDBA defines hearing loss using the ear average for four
frequencies 0.5, 1, 2, and 4 kHz. These differences in the definition of
hearing loss thresholds and used frequencies may cause higher prevalence of
hearing loss cases in the Brazilian and Swedish studies.
Although there is an important number of publications on the
relationship between teaching and classroom acoustics with occurrence of
communicative disorders among teachers, most of them are focused on voice disorders
[23,29-31], with few studies on the
occurrence and consequences of hearing loss among teachers [32,33]. Previous studies on
noise and voice concluded that acoustics and noise conditions are associated
factors for the onset and persistence of voice disorders among teachers [2,29]. One explanation for this association
between noise and voice is the Lombard effect [34],
defined as the modification of the voice production in the presence of noise
due to the masking of voice. Therefore, under noisy conditions, teachers may
tend to increase their vocal effort [35] and
raise their voices to guarantee the success of the communication process, which
may lead to the development of voice disorders [36,37].
Publications on noise and hearing have studied the effect of
noise exposure among music teachers [38-40].
Previous studies have reported mean values of noise levels in occupied
classrooms ranging from 72 dBA [29] to 76
dBA [41] with noise sources inside the
classrooms such as toys and classroom noise during different activities [9,42]. Although these values do not exceed the
permissible exposure limits as currently defined by international standards, 90
dBA for an 8-hour day with a 5 dBA exchange rate (which means that for every
5dBA increase, the amount of exposure time is cut in half), they can affect
hearing functioning and voice production among teachers [43]. Therefore, consistent noise levels inside the classrooms
over time might affect the communication process, as well as the general health
status of teachers [29,42]. Lindblad et al. (2014) reported that teachers showed similar results as
industrial workers for speech recognition in noise and tinnitus, which may
suggest lesions in the inner hair cell area due to exposure to sudden loud
sounds, such as screams of the children [44].
Since hearing is the main tool for receiving verbal information, its
breakdown negatively influences the teaching-learning process. As a result, teachers need to adjust
their teaching strategies to maintain an adequate learning environment inside
the classrooms. Moreover, previous authors have reported that work-related noise may contribute to
physical and mental health disorders in teachers [45].
Concerning
the third aim of this study, our findings indicated that voice disorders,
although more frequent among teachers that have contacted the Colombian NBDA for
follow-up, were identified by the members of the Colombian NBDA with lower percentage
of handicap compared with hearing problems. In this study, the members of the
NBDA determined that voice disorders did not interfere strongly with the daily
activities of teachers. The average handicap percentage for teachers with voice
disorders was 3%, whereas for hearing problems was 6%. Even though the voice is
a teacher’s primary occupational tool, teachers may consider voice disorders to
be a normal part of the health-work process. Therefore, it is common that
teachers accept their voice disorders and continue teaching despite vocal health issues,
which means that the perceived limitation in activity due to voice disorders is
lower than hearing problems. Nevertheless, previous research has reported that
teachers who continue teaching during periods of vocal impairment incur
significant direct and indirect costs due to productivity loss, absenteeism and
use of healthcare system [46].
Moreover,
considering the focus of the evaluation of disability performed by the NBDA, it
seems likely that communication problems have low percentage of disability and
handicap, even though this does not reflect the impact of these problems in
daily life and quality of life. Our results reflect this weakness in the
evaluation process and highlight the need of implement specific protocols to
assess different type of disabilities.
This
study has several limitations. First, there was a limited sample size from
those seeking medical help and being included in the database. Second, this population
was limited further because it included exclusively workers who did not agree
with their initial evaluations and looked for a third-part assessment by the
NBDA, which hampers the ability to generalize the findings. Additionally, as
with any large-scale data collection and database, analysis and results are
dependent on the criteria and protocols (and compliance to those protocols). Finally,
the study did not include other variables of interest (e.g., level of teaching)
because they were not included in the database, which may limit the possibility
of analyzing other important factors associated with the occurrence of
communication problems among teachers.
In conclusion, while teachers that have contacted the Colombian NBDA for follow-up have a high occurrence of voice disorders, hearing problems is more likely to be stated as a more severe disability than a voice disorder. One possible explanation is that teachers who contacted the Colombian NBDA for follow-up did continue working even when many symptoms were evident, while hearing problems would prevent a teacher from interacting with students, thereby affecting the teaching-learning process. Nevertheless, with both voice and hearing problems, work performance and social interaction is affected, and therefore quality of life is reduced. For this reason, it is important to design and implement work-based communicative health promotion programs that aim to reduce the high occurrence of voice problems and the high limitation of hearing problems for teachers. A first step for the design of such programs is the definition of an epidemiologic profile of work-related voice disorders among teachers. This profile would help lawmakers and health professionals establish guidelines on the prevention of the most common work-related diseases among teachers. Future research is also needed to clarify the natural variation and work-relatedness of hearing problems among teachers.
References
1. American Speech-Language-Hearing Association (ASHA). Definitions of communication disorders and variations. Maryland: American Speech-Language-Hearing Association; 1993. Doi: https://doi.org/10.1044/policy.RP1993-00208
2. Cantor Cutiva L, Vogel I, Burdorf A. Voice disorders in teachers and their associations with work-related factors: A systematic review. Journal of Communication Disorders. 2013;46(2):143-55. Doi: https://doi.org/10.1016/j.jcomdis.2013.01.001
3. OECD. Education at a Glance 2015: OECD Indicators. Paris: OECD Publishing; 2015.
4. Simberg S, Santtila P, Soveri A, Varjonen M, Sala E, Sandnabba NK. Exploring genetic and environmental effects in dysphonia: a twin study. Journal of Speech, Language, and Hearing Research. 2009;52(1):153-63. Doi: https://doi.org/10.1044/1092-4388(2008/07-0095)
5. Nerrière E, Vercambre M-N, Gilbert F, Kovess-Masféty V. Voice disorders and mental health in teachers: a cross-sectional nationwide study. BMC Public Health. 2009;9(1):370. Doi: https://doi.org/10.1186/1471-2458-9-370
6. Carrillo-Gonzalez, A, Camargo-Mendoza, M, & Cantor-Cutiva, LC.. Relationship between sleep quality and stress with voice functioning among college professors: a systematic review and meta-analysis. Journal of Voice. 2021;35(3):499-e13. Doi: https://doi.org/10.1016/j.jvoice.2019.11.001
7. Carrillo-González A, Atará-Piraquive ÁP. Vocal health and stress: the occupational voice users’ perspective during the COVID-19 pandemic. Revista de Investigación e Innovación en Ciencias de la Salud. 2020;2(2):102-110. Doi: https://doi.org/10.46634/riics.38
8. Garcia Martins RH, Mendes Tavares EL, Lima Neto AC, Fioravanti MP. Occupational hearing loss in teachers: a probable diagnosis. Revista Brasileira de Otorrinolaringologia. 2007;73(2):239-44. Doi: https://doi.org/10.1016/S1808-8694(15)31072-7
9. Sjödin F, Kjellberg A, Knutsson A, Landström U, Lindberg L. Noise exposure and auditory effects on preschool personnel. Noise Health. 2012;14(57):72-82. Doi: https://doi.org/10.4103/1463-1741.95135
10. Yang X, Ge C, Hu B, Chi T, Wang L. Relationship between quality of life and occupational stress among teachers. Public Health. 2009;123(11):750-5. Doi: https://doi.org/10.1016/j.puhe.2009.09.018
11. Cantor Cutiva L, Burdorf A. Factors associated with voice-related quality of life among teachers with voice complaints. Journal of Communication Disorders. 2014;52:134-42. Doi: https://doi.org/10.1016/j.jcomdis.2014.05.003
12. World Health Organization (WHO). International classification of impairments, disabilities and handicaps: a manual of classification relating to the consequences of disease. Geneve: World Health Organization; 1980.
13. Presidencia de la República de Colombia. Decree 1295 of 1994 (Decreto 1295 de 1994). In: Ministerio de Trabajo y Seguridad Social, editor. Bogotá D.C.; 1994.
14. Presidencia de la República de Colombia. Decree 1477 of 2014 (Decreto 1477 de 2014). Bogotá D.C.; 2014.
15. Presidencia de la República de Colombia. Decree 917 of 1999 (Decreto 917 de 1999). Bogotá D.C.; 1999.
16. Rondinelli R, Genovese E, Katz R, Mayer T, Mueller K, Ranavaya M. Guides to the evaluation of permanent impairment. Chicago: American Medical Association press; 2009. Doi: https://doi.org/10.1001/978-1-57947-888-9
17. Maldonado G, Greenland S. Simulation Study of Confounder-Selection Strategies. American Journal of Epidemiology. 1993;138(11):923-36. Doi: https://doi.org/10.1093/oxfordjournals.aje.a116813
18. Cantor Cutiva L, Fajardo A, Burdorf A. Associations between self-perceived voice disorders in teachers, perceptual assessment by speech-language pathologists, and instrumental analysis. International Journal of Speech-Language Pathology. 2016;18(6):550-9. Doi: https://doi.org/10.3109/17549507.2016.1143969
19. Preciado-Lopez J, Perez-Fernandez C, Calzada-Uriondo M, Preciado-Ruiz P. Epidemiological study of voice disorders among teaching professionals of La Rioja, Spain. Journal of Voice. 2008;22(4):489-508. Doi: https://doi.org/10.1016/j.jvoice.2006.11.008
20. Fritzell B. Voice disorders and occupations. Log Phon Vocol. 1996;21(1):7-12. Doi: https://doi.org/10.3109/14015439609099197
21. Pekkarinen E, Himberg L, Pentti J. Prevalence of vocal symptoms among teachers compared to nurses-a questionnaire study. Scandinavian Journal of Logopedics and Phoniatrics. 1992;17:112-7. Doi: https://doi.org/10.3109/14015439209098721
22. Roy N, Merrill R, Thibeault S, Gray S, Smith E. Voice disorders in teachers and the general population: Effects on work performance, attendance, and future career choices. Journal of Speech, Language, and Hearing Research. 2004;47(3):542-51. Doi: https://doi.org/10.1044/1092-4388(2004/042)
23. Cantor Cutiva LC, Burdorf A. Work-related determinants of voice complaints among school workers: An eleven-month follow-up study. American Journal of Speech-Language Pathology. 2016;25(4):590-7. Doi: https://doi.org/10.1044/2016_AJSLP-14-0191
24. Grillo MHM, Penteado RZ. Impacto da voz na qualidade de vida de professore(a)s do ensino fundamental. Pró-Fono Revista de Atualização Científica. 2005;17:311-20. Doi: https://doi.org/10.1590/s0104-56872005000300006
25. Penteado RZ, Pereira IMTB. Qualidade de vida e saúde vocal de professores. Revista de Saúde Pública. 2007;41:236-43. Doi: https://doi.org/10.1590/S0034-89102007000200010
26. Roy N, Merrill R, Thibeault S, Parsa R, Gray S, Smith E. Prevalence of voice disorders in teachers and the general population. Journal of Speech, Language, and Hearing Research. 2004;47(2):281-93. Doi: https://doi.org/10.1044/1092-4388(2004/023)
27. Mattiske J, Oates J, Greenwood K. Vocal problems among teachers: a review of prevalence, causes, prevention, and treatment. Journal of Voice. 1998;12(4):489-99. Doi: https://doi.org/10.1016/S0892-1997(98)80058-1
28. Hunter EJ, Tanner K, Smith ME. Gender differences affecting vocal health of women in vocally demanding careers. Logopedics Phoniatrics Vocology. 2011;36(3):128-36. Doi: https://doi.org/10.3109/14015439.2011.587447
29. Cantor Cutiva L, Burdorf A. Effects of noise and acoustics in schools on vocal health in teachers. Noise Health. 2015;17(74):17-22. Doi: https://doi.org/10.4103/1463-1741.149569
30. De Medeiros A, Barreto S, Assuncao A. Voice disorders (dysphonia) in public school female teachers working in Belo Horizonte: prevalence and associated factors. Journal of Voice. 2008;22(6):676-87. Doi: https://doi.org/10.1016/j.jvoice.2007.03.008
31. Ilomaki I, Leppanen K, Kleemola L, Tyrmi J, Laukkanen A, Vilkman E. Relationships between self-evaluations of voice and working conditions, background factors, and phoniatric findings in female teachers. Logopedics Phoniatrics Vocology. 2009;34(1):20-31. Doi: https://doi.org/10.1080/14015430802042013
32. Servilha EAM, Delatti MdA. Noise perception in the workplace and auditory and extra-auditory symptoms referred by university professors. Jornal da Sociedade Brasileira de Fonoaudiologia. 2012;24(3):233-8. Doi: https://doi.org/10.1590/S2179-64912012000300008
33. Jiang T. Can noise levels at school gymnasia cause a hearing loss: A case study of a physical education teacher. Journal of the Acoustical Society of America. 1997;101(5):3069. Doi: https://doi.org/10.1121/1.418754
34. Lane H, Tranel B. The Lombard Sign and the Role of Hearing in Speech. Journal of Speech and Hearing Research. 1971;14(4):677-709. Doi: https://doi.org/10.1044/jshr.1404.677
35. Hunter EJ, Cantor-Cutiva LC, Van Leer E, Van Mersbergen M, Nanjundeswaran CD, Bottalico P, et al. Toward a Consensus Description of Vocal Effort, Vocal Load, Vocal Loading, and Vocal Fatigue. Journal of Speech, Language, and Hearing Research. 2020;2:509-532. Doi: https://doi.org/10.1044/2019_JSLHR-19-00057
36. Vilkman E. Voice problems at work: A challenge for occupational safety and health arrangement. Folia Phoniatr Logop. 2000 Jan-Jun;52(1-3):120-5. Doi: https://doi.org/10.1159/000021519
37. Zollinger SA, Brumm H. The evolution of the Lombard effect: 100 years of psychoacoustic research. Behaviour. 2011;148(11-13):1173-98. Doi: https://doi.org/10.1163/000579511X605759
38. Cutietta R, Klich R, Royse D, Rainbolt H. The Incidence of Noise-Induced Hearing Loss among Music Teachers. Journal of Research in Music Education. 1994;42(4):318-30. Doi: https://doi.org/10.2307/3345739
39. Behar A, MacDonald E, Lee J, Cui J, Kunov H, Wong W. Noise exposure of music teachers. Journal of Occupational and Environmental Hygiene. 2004 Apr;1(4):243-7. Doi: https://doi.org/10.1080/15459620490432178
40. Chesky K. Schools of music and conservatories and hearing loss prevention. International Journal of Audiology. 2011;50(sup1):S32-S7. Doi: https://doi.org/10.3109/14992027.2010.540583
41. Ramig LO, Verdolini K. Treatment Efficacy: Voice Disorders. Journal of Speech, Language, and Hearing Research. 1998;41(1):S101-S16. Doi: https://doi.org/10.1044/jslhr.4101.s101
42. McAllister AM, Granqvist S, Sjölander P, Sundberg J. Child voice and noise: a pilot study of noise in day cares and the effects on 10 children's voice quality according to perceptual evaluation. Journal of Voice. 2009;23(5):587-93. Doi: https://doi.org/10.1016/j.jvoice.2007.10.017
43. Occupational Safety and Health Administration (OSHA). 1910.95, Occupational noise exposure. In: United States Department of Labor, editor. Washington DC: United States Department of Labor; 2011.
44. Lindblad A-C, Rosenhall U, Olofsson Å, Hagerman B. Tinnitus and Other Auditory Problems-Occupational Noise Exposure below Risk Limits May Cause Inner Ear Dysfunction. PloS one. 2014;9(5):e97377. Doi: https://doi.org/10.1371/journal.pone.0097377
45. Sala E, Rantala L. Acoustics and activity noise in school classrooms in Finland. Applied Acoustics. 2016;114:252-9. Doi: https://doi.org/10.1016/j.apacoust.2016.08.009
46. Cantor Cutiva L, Burdorf A. Medical Costs and Productivity Costs Related to Voice Symptoms in Colombian Teachers. Journal of Voice. 2015;29(6):776.e15-.e22. Doi: https://doi.org/10.1016/j.jvoice.2015.01.005
Additional information
How to
cite: Cantor-Cutiva, Lady Catherine; Cuervo-Diaz, Diana Elizabeth;
Hunter, Eric J.; Moreno-Angarita, Marisol. (2021). Impairment, disability, and
handicap associated with hearing problems and voice disorders among Colombian
teachers. Revista de Investigación e Innovación en
Ciencias de la Salud. 3(1): 4-21. https://doi.org/10.46634/riics.48
Editor: Jorge
Mauricio Cuartas Arias, Ph.D., https://orcid.org/0000-0001-9007-713X
Coeditor: Fraidy-Alonso Alzate-Pamplona, MSc., https://orcid.org/0000-0002-6342-3444
Copyright: © 2021. Fundación Universitaria María Cano. The Revista de Investigación e Innovación
en Ciencias de la Salud provides open access to all its
content under the terms of the Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0).
Conflicts of Interest: The authors have declared that no competing interests exist.
Data Availability Statement: All relevant data is in the article. For more detailed
information, write to the Corresponding Author.
Funding: None. This research did not receive any specific grants from
funding agencies in the public, commercial, or non-profit sectors.
Disclaimer: The content of this article is the sole responsibility of the
authors and does not represent an official opinion of their institutions or the
Revista de Investigación e Innovación en Ciencias de la
Salud.
Correspondence: Lady Catherine
Cantor-Cutiva. Ciudadela Universitaria, Carrera 30 Calle 45. Facultad de
Enfermería, Room 207. Telephone:
+57 1 316500 ext 17081. Email: lccantorc@unal.edu.co
Alternative link
https://revistas.fumc.edu.co/ojs/index.php/RCMC/article/view/48 (html)