



Artículo Original
The music therapy and harm model (MTHM). Conceptualizing harm within music therapy practice
ECOS - Revista Científica de Musicoterapia y Disciplinas Afines
Universidad Nacional de La Plata, Argentina
ISSN-e: 2718-6199
Periodicidad: Semestral
vol. 6, núm. 1, e003, 2021
Recepción: 22 Febrero 2021
Aprobación: 01 Abril 2021

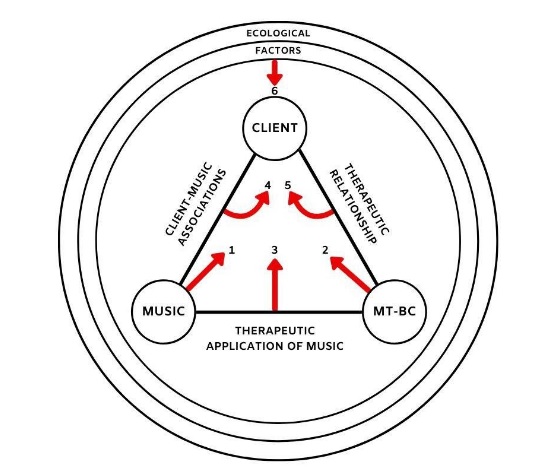
Resumen: Los musicoterapeutas clínicos e investigadores discuten ampliamente los beneficios terapéuticos de la música, pero han pasado por alto en gran medida la posibilidad de que surjan daños durante las sesiones de musicoterapia. Este tema importante puede pasarse por alto debido a su complejidad. Definir y comprender los efectos negativos de la música y la musicoterapia son tareas difíciles. Sin embargo, la musicoterapia puede progresar en varios temas (por ejemplo, reconocimiento gubernamental, estándares educativos) al examinar los efectos potencialmente dañinos de las intervenciones basadas en la música. Las menciones al daño dentro de la literatura de musicoterapia son irregulares e imprecisas, quizás porque el campo carece de una estructura teórica para organizar este complicado tema. Este artículo presenta el Modelo denominado “Music Therapy and Harm Model” (MTHM), el cual tiene como objetivo conceptualizar seis fuentes potenciales de daño dentro de la práctica clínica de la musicoterapia. Específicamente, estas fuentes potenciales incluyen 1) la música presentada, 2) el musicoterapeuta, 3) la aplicación terapéutica de la música, 4) la relación terapéutica, 5) las asociaciones musicales específicas del cliente y 6) los factores ecológicos. Este documento ilustra cada fuente ejemplificando cada posible daño físico o psicológico. Además, se teoriza que estos mismos factores actúan como elementos protectores que permiten a los musicoterapeutas remediar casos de daño y promover la resiliencia del cliente frente a las experiencias negativas de la musicoterapia. El MTHM se conceptualiza aún más con una breve revisión de la literatura sobre el daño dentro de la práctica de la musicoterapia, junto con la investigación relacionada en psicoterapia. Finalmente, este artículo expone las implicaciones clínicas, educativas, de promoción, de investigación y globales del MTHM.
Palabras clave: Musicoterapia, daño, efectos negativos, eventos adversos, modelo teórico.
Abstract: Music therapy researchers and clinicians widely discuss music’s therapeutic benefits, but have largely overlooked the potential for harm to arise within music therapy sessions. This important topic may be neglected due to its complexity; defining and understanding negative effects of music and music therapy are difficult endeavors. However, the music therapy profession may make progress on several professional issues (e.g., governmental recognition, educational standards) by examining the potentially harmful effects of music-based interventions. Mentions of harm within music therapy literature are irregular and imprecise, perhaps because the field lacks a theoretical structure to organize this complicated subject. This paper presents the Music Therapy and Harm Model (MTHM), which aims to conceptualize six potential sources of harm within clinical music therapy practice. Specifically, these potential sources include 1) the music presented, 2) the music therapist, 3) the therapeutic application of music, 4) the therapeutic relationship, 5) client-specific music associations, and 6) ecological factors. This paper illustrates each source with examples of either physical or psychological harm. Furthermore, these same factors are theorized to act as protective elements that allow music therapists to remediate instances of harm and promote client resilience in the face of negative music therapy experiences. The MTHM is further conceptualized with a brief literature review surrounding harm within music therapy practice, along with related research in psychotherapy. Finally, this article lays out the clinical, educational, advocacy, research, and global implications of the MTHM.
Keywords: music therapy, harm, negative effects, adverse events, theoretical model.
Music therapists are primarily concerned with the beneficial application of music to advance or support a client’s therapeutic goals. The positive effects of music interventions for diverse clinical populations are well-established. However, if music can help clients, then the reverse principle is also possible: music may be harmful to clients. The same power of music to influence people’s behaviors, thoughts, and emotions may also become a source of distress if not insightfully understood or monitored. The concept that music or (by extension) a music therapy session may produce negative or undesirable responses has not been widely addressed in the literature.
Researchers have acknowledged the potentially negative impact of music across diverse settings. For instance, evidence exists that music listeners may use music maladaptively for emotion regulation. Several individual factors may increase this negative use of music including gender (Carlson et al., 2015) and social listening context (Garrido et al., 2017). Similarly, Saarikallo et al., (2015) developed the Healthy-Unhealthy Uses of Music Scale and found a relationship between adolescent listeners’ musical engagement and reports of depressive symptoms. Some of the most extreme evidence for music’s ability to harm people comes from academic reviews of detention practices by the United States military during the Afghanistan and Iraq wars in the early 2000s. Detainees from Muslim-majority countries were subjected to intensely loud, Western music for up to 18 hours a day to procure information from prisoners (Cusick, 2008). According to research outlined in government documents, the intense music was meant to either overload or deprive the prisoners’ sensory systems in order to induce a dissociated psychological state (Conroy, 2000; McCoy, 2006; Otterman, 2007). Although such an extreme use of music would not occur in a clinical setting, these torture scenarios are start illustrations of how music may inflict harm.
Several music therapists have mentioned specific examples of how music may become a source of distress. Roskam (1993) focused on music’s classification as a potentially damaging stimulus arising from cultural and personal associations of music or music’s psychophysical properties. Additionally, Gattino (2015) outlined several potential negative effects of music including altered states of awareness, extended repetition of music, and listening to music associated with a negative life event. Abbott (2005) examined the potential for negative experiences to arise within a single therapeutic approach, the Bonny Method of Guided Imagery and Music (GIM). Abbott found that experiences that clients deemed as “negative” were associated with music that was incongruent to themselves, or impacted them in a way that was uncomfortable or undesired.
More generally, Gardstrom (2008) questioned the assertion that music therapy is a “non-invasive” or “non-threatening” modality and argued that music’s power to beget therapeutic change is partly due to its physical or psychological pervasiveness. The most direct argument for music therapists to understand harm may be presented by Isenberg (2012) who wrote: “We are obliged to define ourselves as those who can do good, not because of the benign or therapeutic nature of our tool, but because our interventions have the power to do harm” (p. 70). Isenberg discussed general examples of therapeutic harm (e.g., the poor evaluation of needs, the therapist imposing their will onto patients) and then explored examples of harm specific to music therapy practice (e.g., poor selection of music or instruments, the music therapist’s inappropriate control of patient music, or adverse structuring of musical elements).
Although scholars have initiated a discussion, the music therapy field as a whole lacks a comprehensive vocabulary or way to conceptualize music and harm within a clinical context. The confusion surrounding harm and music within its clinical applications may exist for several reasons. First, the detection of harm within therapeutic settings is complicated. Hatfield et al., (2010) found that therapists on their own may not reliably detect when a client’s progress deteriorates. Further, several confounding factors exist that make detecting instances of therapeutic harm challenging including client progress in treatment, a lack of measurement tools for negative outcomes, or even more fundamentally, an agreed-upon definition of harm among professionals (Dimidjiam y Hollon, 2010; Linden, 2013; Rozental et al., 2018).
Thus, this paper has two purposes: 1) to propose preliminary definitions of harm relevant to music therapy, and 2) to introduce the Music Therapy and Harm Model (MTHM) as a way to conceptualize potential sources of harm within music therapy. Of note, the MTHM has a relatively narrow scope and is intended to be applied to clinical music therapy practice as defined and regulated by a formal organization (e.g., the American Music Therapy Association in the United States). The definitions of harm and the MTHM presented are not meant to be equilaterally applied to other uses of music for health purposes (e.g., music thanatologists, traditional uses of music for healing).
Defining terminology related to harm
Although music therapists are obligated to understand and address harm when it occurs, the field lacks clinical terminology to describe harm. Defining clinical harm is difficult for several reasons. First, the term harm is itself vague. What type of therapy can “harm” a client? What types of harm are possible? Clinicians’ opinions may also differ on what constitutes harm based on their philosophical orientation or clinical expertise. Few music therapy resources exist to address these issues. Currently, no explicit definition of harm was found by this author in the American Music Therapy Association (AMTA) and Certification Board for Music Therapists (CBMT) documents mentioned in this paper, nor in reviewed literature. The field of psychotherapy may provide a starting point to defining harm. Dimidjian and Hollon (2010) outlined basic characteristics of harmful treatments including a causal effect in which outcomes are worse than if the treatment had not been provided. In addition, they clarified that a harmful treatment is more than simply unhelpful — it can result in injury or damage to the client.
Several terms related to harm should be outlined before presenting this paper’s definitions of harm. One term used in the psychotherapy literature is a negative effect, which comprises negative outcomes and experiences the client attributes to therapeutic treatment, and may describe potentially harmful events (Barlow, 2010; Rozental et al., 2018). Negative effects include experiences related to therapy that are subjectively deemed negative or unwanted, and may be relatively common in therapeutic settings. Rheker et al., (2017) investigated rates of negative effects (i.e., negative patient experiences or changes associated with therapy) in psychiatric patients and found that 45 to 58% of psychiatric patients reported at least one negative effect during treatment. Examples of patient-perceived negative effects included feeling down more often or having difficulty making decisions independently, without help from the therapist. Although these negative effects may not result in “harm” directly, the researchers asserted that it is not uncommon for patients to have negative experiences when engaging in therapy. As such, negative experiences may not be inherently harmful and may occur within significant therapeutic events that move the client closer to reaching their goal (Linden y Schermuly-Haupt, 2014). For example, crying in therapy is not often experienced as pleasant, but can still serve as a cathartic release that allows the client to process a painful event. Negative effects may not always be harmful, but harm always arises from a negative effect. A related therapeutic term is a contraindication, which can be understood as the individual conditions of a case that make an adverse reaction to treatment highly probably (Linden, 2013).
This paper theorizes that the client may experience harm in one of two ways: physically or psychologically. Physical and/or psychological harm may be experienced by the client in response to any of the six MTHM sources outlined in later sections. Physical harm is defined as a negative effect not in service of the therapeutic objective arising from a physiological mechanism or system. Physical harm could manifest as a negative change in the client’s body, brain, or other physiological structure. Such physical harm could potentially be measured via heart rate, respiration rate, hormone levels, client pain ratings, and/or brain activity. More specific examples physical harm might include bodily injury, an increase in pain, the creation of maladaptive neural connections, or sensory regulation issues. Similarly, psychological harm is defined as a negative effect not in service of the therapeutic objective arising from a psychological mechanism or system. Psychological harm could potentially be measured via client self-report, observation of client behavior, or distress portrayed in clinical documents such as the therapist’s notes, a client’s writings, or a client’s artistic materials. Specific examples of psychological harm might include emotional dysregulation, mental rumination, feelings of danger, a decrease in a client’s self-efficacy, maladaptive perceptions of reality, or the triggering of symptoms associated with a mental health diagnosis.
Additionally, harm may occur on different continuums of time and intensity. Along the time continuum of harm, a client may experience harm before, during, or after a session occurs. An example of harm occurring before the session is anticipatory anxiety prior to a session. Additionally, the effects of harm may continue after a session ends or manifest after a session has occurred. For example, a client may experience injuries after session if not provide adequate rest breaks between music-guided movement activities (e.g., Patterned Sensory Enhancement). Along the intensity continuum of harm, clients can experience the strength of the harm to be of very high intensity that may lead to prolonged physical or psychological trauma that extends to situations beyond the therapeutic music experience. On the other hand, clients may experience harm to a degree of lesser intensity, that is able to be remedied immediately once the harm is brought to the attention of the music therapist.
These definitions of harm are not intended to prevent or dissuade therapists from introducing meaningful risks or challenging experiences into clinical sessions as planned and monitored by a music therapist operating within their scope of practice. Oftentimes, a client’s progress toward their clinical goals requires thoughtful interactions between the client, therapist, and music which may result in negative feelings, mild distress, or otherwise uncomfortable experiences that ultimately lead to positive benefits (Gardstrom, 2008). This paper’s intent is not to discourage music therapists from introducing these types of intentional and clinically-monitored experiences into a session. Doing so would only perpetuate incorrect and shallow assumptions that music and music therapy is always a helpful and positive experience (Edwards, 2011). Rather, this paper explores how music therapists might conceptualize clinical experiences that are contraindicated from best practice, as determined by client needs, research, and clinician expertise (Abrams, 2010). Thus, the intention for the above definitions and its qualifiers is to provide a starting point for delineating potential sources of harm.
Rationale for the music therapy and harm model
Identifying how harm might arise in music therapy sessions is warranted for several reasons. Primarily, if harm is not recognized as a possible outcome of music therapy, then this issue cannot be prevented or addressed, which may leave consumers of music therapy at higher risk of physical and/or psychological harm. For examples, clients exposed to detrimental conditions within a music therapy session could regress in their goals or be left with short- or long-term consequences to their physical and/or mental health. Harm is further implicated in several documents regulating clinical music therapy practice in the United States. First, the Scope of Practice (AMTA y CBMT, 2015) is a document outlining the responsibilities of a credentialed music therapist and explicitly states that trained and competent music therapists recognize the potential for harm present in music, verbal, or physical interventions. Additionally, the Scope of Practice states that music therapists should be aware of contraindications to specific health conditions or other client factors. Second, the AMTA Code of Ethics (2019) dictates that music therapists protect the client’s right to safety. Finally, the AMTA’s Standards of Clinical Practice state that music therapists should make every effort to “ensure safe and quality client care” (4.1.3; AMTA, 2013a).
The topic of harm also holds professional relevance to music therapists through advocacy initiatives. Advocacy efforts to protect consumers in the United States from potential harm are already well-underway through the American Music Therapy Association’s (AMTA) and the Certification Board for Music Therapists’ (CBMT) State Recognition Operational Plan (CBMT, n.d.). This joint initiative advocates for governmental recognition of the music therapy profession. As listed in the CBMT website, one purpose of this plan is to protect clients from potential harm by unqualified individuals. Per these documents, music therapists are commissioned to maximize clinical benefits and minimize harm. However, without understanding how harm can occur, clinicians may not be able to foresee and respond effectively when adverse reactions arise. Thus, this paper seeks to begin a professional discussion by presenting a common way to conceptualize this complex topic.
The music therapy and harm model
The Music Therapy and Harm Model (MTHM) is a means for conceptualizing potential sources of physical and/or psychological harm in music therapy practice. The model was first conceptualized in response to my participation in legislative advocacy efforts in 2015, during which I was unable to articulate to my state representative how a music therapy license would protect consumer safety. The model in its current form arose from my bottom-up observations and work within several distinct clinical settings (e.g., medical hospital, older adult care facility, behavioral health) as well as professional conversations amongst peers and mentors. Early versions of the model were refined after collecting feedback following its presentation at national and regional conferences in the United States (Murakami, 2018; Murakami y Goldschmidt, 2017), and in the AMTA Pro Podcast (Murakami y Goldschmidt, 2018).
The MTHM theorizes that harm may arise from the components present in music therapy sessions (i.e., the client, the music, the music therapist, session context) and the dynamics connecting these components. Altogether, these components and their subsequent interactions are conceptualized into the MTHM triangle (Figure 1). These components and their interactions have been identified as defining features of music therapy, most prominently in Bruscia’s (2014) Client-Music-Therapist Constellation. Readers should note that any of these components or their interactions can also serve as points of protection to mitigate harm. Although the model will be described in terms of how harm may be induced, the protective potential of the MTHM components and interactions will be explored in later sections of this paper.
At the top of the MTHM triangle is the client, who is a recipient of therapy who needs or seeks the help of the music therapist to address a concern or goal related to the client’s health (Bruscia, 2014). The MTHM does not conceptualize the client as a potential source of harm. Although the client is usually a willing participant who has efficacy and autonomy, it is the therapist (rather than the client) who is responsible for maintaining safety within the therapeutic space.
The Music Therapy and Harm Model (MTHM)
Harm arising from a music stimulus (1).
Music is the component of the MTHM represented in the triangle’s lower left corner. Music in the context of a music therapy session refers to any acoustic event presented or facilitated with clinical intent. The music component may consist of recorded or live pieces of music, music improvised by the therapist and/or client, or individual elements inherent to the therapeutic music. The potential for harm arises from the music (1) when the psychoacoustic energy (i.e., the vibrations, sensations, or perceptions a client receives from a musical stimulus) causes physical or psychological distress for the client that is not in service of a therapeutic objective.
Even when used as a tool for therapeutic change, music may still be an unintended source of harm. For example, a child on the autism spectrum with sensory regulation issues may not be able to tolerate overly complex music (Kalas, 2012) or certain timbres due to atypical neurological organization of the auditory system. Extended exposure to overstimulating music may cause dysregulation that would in turn cause psychological or physical discomfort. Music may also induce musicogenic seizures, which can result from a variety of auditory stimuli including musical content, specific musical elements, or emotional associations with the offending music (Kaplan, 2003). For epileptic clients, these types of seizures may result in physical harm via neurologic damage to the patient’s brain or result in bodily incapacitation. A third examples of music acting as a source of harm may include inappropriately complex music administered to infants in the neonatal intensive care unit (Lowey et al., 2013).
Harm arising from the music therapist (2).
The music therapist (2) within the MTHM triangle is represented in the lower right corner. The music therapist is an accredited music therapy professional who has completed required educational and clinical training standards. The music therapist’s role is to competently and ethically facilitate the client’s journey through the clinical process within their scope of practice. Additionally, the music therapist is responsible for maintaining physical and psychological safety in the therapeutic space. The potential for harm arises if the music therapist possesses qualities or lacks acumen that lead to poor decision-making or responsiveness during the clinical process. These therapist-centric qualities may include inadequate clinical training, practicing outside one’s scope of practice, or personal elements such as personality traits or improper motivations that could result in actions causing harm to the client. Put another way, harm can occur when the music therapist lacks self-awareness, knowledge, or judgment leading to non-musical decisions that compromise the client’s safety.
For example, the risk of physical harm may increase if a music therapist fails to fully educate themselves before working with a client with Parkinson’s disease (PD) for the first time. If the music therapist lacks understanding that postural instability is a cardinal feature of PD and plans movement activities that involve standing without ensuring adequate support staff are present, then the client may be at a greater risk of physical harm via falling due to the therapist’s poor planning. The music therapist may also embody a source of harm if they make detrimental decisions such as censoring a client’s access to their own preferred music based on the music therapist’s personal beliefs, rather than on a therapeutic rationale (Joplin y Dvorak, 2016). Similarly, a music therapist who avoids seeking feedback or supervision in regards to challenging clinical situations may increase the clients’ subsequent risk of harm. If the therapist does not recognize the need for self-reflection and external feedback, then patterns of unhelpful or potentially harmful micro-interactions may compound and stymie the treatment (Nutt Williams, 2008). Finally, if an unqualified music therapist attempts an advanced level of therapeutic work, such as a music therapist attempting to do psychodynamic Analytical Music Therapy techniques without additional training, then the client may be at a greater risk of harm.
Harm arising from the application of music interventions (3)
The therapeutic application of music (3) serves as the bottom side of the MTHM triangle, connecting the music and the music therapist components. Music-based interventions are planned and facilitated by the music therapist to support client progress toward clinical goals. Such experiences led by the music therapist may include a) standardized protocols, b) thoughtfully planned, but less specific interventions, or c) responsive improvisation. Harm may arise from the therapeutic application of music if the music therapist makes poor musical decisions during a session, or if they fail to respond effectively to a client’s negative reaction to the therapeutic music experience (TME).
Incorrect or unmonitored application of a TME by the music therapist may additionally harm a client if a contraindication regarding a music-based intervention is disregarded. For example, a music therapist implementing Melodic Intonation Therapy (MIT) with a patient with expressive aphasia should not continue to press the client to repeat incorrect words or errors, per protocol instructions (Thaut et al., 2014). Disregarding this contraindication may result in physical harm because the client may develop maladaptive neuroplasticity (i.e., plastic changes in the brain that lead to dysfunction) that permanently impacts their communication abilities. Repetitive behaviors have been shown to induce altered sensory perceptions, motor coordination, and chronic pain in musicians (Altenmüller y Furuya, 2017). Similar changes resulting from TMEs still need to be verified, but are theoretically possible. Another contraindication of music therapy involves the Multimodal Stimulation Protocol used with premature infants. Specifically, if an infant shows signs of overstimulation (e.g., hiccoughs, grimacing, or clinched eyes) in response to auditory, tactile, or vestibular stimulation, then that type of stimulation is contraindicated and should be discontinued (Standley y Walworth, 2010).
Harm arising from the therapeutic relationship (4).
The therapeutic relationship (4), is comprised of the interactions between the client and music therapist, and is the fourth point at which harm can occur. Defined as close, trustworthy, and personal relations between the therapist and client, the therapeutic relationship provides a non-judgmental space for client self-exploration (Yalom y Leszcz, 2015). Client-therapist interactions are the foundational element of music therapy and is one of the strongest predictors of successful therapeutic outcomes (Lambert y Barley, 2001). Still, an inherent power imbalance exists between the therapist and client within the therapeutic relationship that should be acknowledged. The therapeutic relationship is non-reciprocal. That is, the client makes themselves vulnerable within the therapeutic relationship at a level not matched by the therapist (Bruscia, 2014). This power differential is not necessarily viewed as inherently damaging or harmful (Gutheil y Brodsky, 2008; Pope y Vasquez, 2007), although some scholars believe power issues should be attended to and reduced to foster more authentic relationships (Proctor, 2002).
Harm may arise from unhealthy or inappropriate client-therapist interactions within the therapeutic relationship. For example, unresolved transference or countertransference may introduce a hazardous dynamic that negatively impacts a client’s health. If unresolved emotions or an undesirable power dynamic between the client and therapist exist, then therapeutic progress and client welfare could be negatively impacted. Further, a therapist may exploit their power in a way that results in verbal, emotional, financial, or sexual abuse (Garrett y Davis, 1998; Gartrell et al., 1986). Such interactions violate ethical boundaries and are often detrimental to clients. Other, less dramatic, but potentially harmful events within this realm include: accepting gifts, becoming friends with clients on social media, or dual relationships between clients and therapists that violate ethical standards. Clearly, therapist-client interactions can be a potent source of harm.
Harm arising from client associations with music (5).
The client-music associations (5) create the left side of the MTHM triangle, which connects the client and music components. This interaction is characterized by the client’s extra-musical associations to the music presented in the therapeutic session including, but not limited to: conditioned responses, preferences, emotional associations with specific musical elements (e.g., the lyrics, an instrument) or knowledge about the music (e.g., the historical context, the musical artist). Harm may arise when a client’s extra-musical associations produce a negative psychological or physical response that is beyond the scope of the session’s therapeutic objective. Metaphorically similar to how this left side of the triangle is not in direct contact with the music therapist corner of the MTHM triangle, these client-music associations are the least likely to be under the direct control of the music therapist and may arise unexpected during treatment. Still, the music therapist is responsible for assessing, monitoring, and addressing the client-music associations as they occur.
For example, a music therapist working with a client with substance use disorder may unintentionally present a song the client played during prior substance use episodes. The client’s resulting craving may cause emotional, cognitive, or physical distress due to the client’s history and conditioned response paired with the music (Short y Dingle, 2016). Other examples of harm arising from client-specific associations with music include the use of acoustic timbres that trigger traumatic memories (e.g., the use of an ocean drum with a client who was sexually abused in the shower), or negative experiences with imagery in response to music (Abbott, 2005).
Harm arising from ecological factors (6).
The final theorized source of harm, ecological factors (6), are represented by three concentric circles surrounding the triangle created by the client, music therapist, and music components. These three outer circles represent the micro-, meso-, and macro-dimensions that encompass a broad context of physical, social, cultural, and historical aspects within in which the music therapy session occurs. These three levels are adapted from Bronfenbrenner’s ecological theory of development (Bronfenbrenner y Morris, 2007). These ecological factors are always present in the session, but may not be under the music therapist’s direct control (nor, in the music therapist’s conscious awareness at times). However, these factors often dictate the client outcomes in music therapy due to the reciprocal relationship between musicking and context (McFerran y Saarikallo, 2014). These ecological factors also include the history underlying the client’s culture-specific associations with musical elements, repertoire, and performance settings.
The innermost circle represents micro-ecological factors including the immediate session environment such as the physical space the session is held in, the time of the session, and other people present (e.g., other clients, other staff members). Next, meso-ecological factors influence the session on a broader scale including the client’s cultural background and identity. Race, gender, socioeconomic status, disability, the client’s life circumstances, and the therapist’s cultural background and identity are included in these meso-ecological factors. Macro-ecological factors include the broadest contexts at play at a societal level including the ideologies and attitudes of the larger culture, as well as systems that impact the client’s ability to access services.
Harm may arise from these ecological factors when the music therapist fails to recognize or appropriately respond to client distress resulting from the contextual interactions that influence the client’s experiences in session. Examples of potential harm at the micro-level may include a session space that is physically unsafe or the music therapist failing set or enforce ground rules to promote safe interactions among all group participants. Moving outward, the meso-level may produce harm as related to the interactions between the therapist and client’s viewpoints, biases, identities, and life circumstances. These intersections include, but are not limited to race, gender, sexual orientation, and/or religious affiliation and may impact the music therapist’s decision making and/or the therapeutic relationship. Some examples of meso-level harm are a music therapist violating a taboo in the client’s culture (e.g., a female music therapist singing for a male Orthodox Jewish client) or misattributing challenging client behaviors due to therapist bias, rather than taking extenuating circumstances in the client’s daily life into account such as a medication change or a life transition.
At the outermost circle, examples of macro-level harm that may occur include the negative physical and/or psychological impact of racism, sexism, ableism, or other systemic forces of oppression that arise in a therapy session (Hadley, 2013; Leonard, 2020). Although music therapists often discuss the need for cultural sensitivity, the importance of this topic is further highlighted in light of its potentially harmful impact on the music therapist’s efficacy. As such, music therapists need to develop a holistic responsiveness to cultural issues and power differences that inevitably arise within the clinical space. The MTHM can and should be subject to continued discussion between scholars with diverse viewpoints to ensure that it does not unintentionally reinforce harmful ideologies.
Summary of MTHM components as potential sources of harm
To summarize, the Music Therapy and Harm Model (MTHM) acknowledges six potential sources of harm in music therapy sessions: 1) the music presented, 2) the music therapist, 3) the therapeutic application of music, 4) the therapeutic relationship, 5) client-music associations, and 6) ecological factors. It is important to acknowledge that all the components making up the model are always present in a music therapy session and therefore inextricably tied together. Furthermore, each of the six sources must be considered in the context of an individual client’s clinical needs, diagnoses, personal history, and cultural ties. This writer acknowledges that harm may look different across various areas or levels of practice, and that real-life examples of harm may be rooted in more than one MTHM source. Delineating exact sources of harm is a complicated in real-life scenarios.
Complicating matters further, improper or unfavorable clinical contexts do not ensure that harm will actually happen. It is possible that a client does not experience harm in a given scenario, even if similar conditions are harmful to another client. Deciding whether harm has occurred and the appropriate actions for remediation should be addressed on a case-by-case basis, in close consultation with the client(s) involved. Credentialed music therapists by themselves may not be able to recognize inadvertent harm they allow or cause. Still, they have the responsibility to listen to, reflect on, and make right the reasonable claims of harm brought to their attention.
Implications of the music therapy and harm model
Clinical implications
Defining and conceptualizing harm raises some potentially uncomfortable feelings for music therapists. It is possible that most, if not all clinicians have at some point caused or allowed harm to occur within a session by this paper’s definitions of harm. To reiterate, the purpose of the MTHM is to articulate and describe potential harm in music therapy practice, not to blame or attack any individual clinician’s practice. Speaking from this writer’s personal experience, coming to terms and being accountable to the fact that oneself has probably caused or allowed harm at some point is a process that involves introspection and acceptance in order to move from a defensive stance to an increasingly aware outlook on one’s own actions as a music therapy professional.
If harm’s prevalence is potentially so common, what can be done to systemically address and remediate harm when it happens? Although the MTHM presents six potential sources of harm, the likelihood of all six sources arising simultaneously is very low. Ideally, music therapists would recognize and respond to client distress by addressing, minimizing, or eliminating the offending source(s) of harm as identified within the MTHM. Hence, a breakdown in one MTHM component’s efficacy might be buffered by strengths of the non-offending components. In other words, harm can be minimized via competent clinical practice when the integrity of one MTHM component is compromised.
One broad solution to reducing harm may involve more opportunities for critical self-examination by music therapists. This paper theorizes that several sources of harm are closely connected to the individual therapist and their decision-making process. A music therapist who lacks self-awareness and fails to examine their own roles and biases may increase the risk of harm to their clients. These discussions about self-awareness could be highlighted in clinical training programs, formal and informal supervision settings, and continuing education opportunities. A more immediate line of defense against potential harm is the music therapist closely monitoring and responding to session events. The following four steps outline one sequence of actions music therapists might implement to minimize harm: 1) vigilant observation and verification of client responses in session, 2) recognition of client distress, 3) identification of the distress source within the MTHM, and 4) responsive modification of MTHM components under the music therapist’s control to minimize distress and process negative experiences.
First, the clinician should consistently monitor the client’s responses in the session. These observations encompass a client’s behaviors, verbalizations, and/or the content of clinical materials (e.g., composed lyrics, drawings). In some cases, the client may not be forthcoming with their negative experiences within a session. Thus, the music therapist should make appropriate efforts to verify that a client is having a therapeutically-meaningful experience (whether positive or negative) and ask the client directly, if needed. Second, the clinician should recognize client-specific signs of distress by drawing upon their training and clinical experience. Once a sign of distress is observed, the clinician should identify which of the six MTHM components is most likely responsible. If possible, this identification should be accompanied with insight into why the client is having a distressed response. Finally, the clinician should respond to the distress by appropriately modifying the MTHM components to better support the client’s immediate needs. For example, the music therapist may reduce or eliminate the source of distress while dynamically re-balancing the salience of the other MTHM components in a way that serves the client’s well-being.
These four steps to minimize harm can be illustrated in the following example. Imagine a music therapist is playing a “Name That Tune” game with recorded music with an adolescent in an inpatient psychiatric setting as a closing “reward” for the client’s participation in an individual session that focused on practicing coping skills and mindfulness. The music therapist shuffles a playlist of popular music and an upbeat party song begins, but the music therapist observes the client tensing their body and averting their eye gaze. This sudden change in the client prompts the music therapist to verbalize their observations and ask how the client is doing. The client then becomes tearful and responds that the song being played reminds them of a friend who recently committed suicide. The music therapist asks the client if they would like the music to be turned off before fading out the music and modeling deep breathing, all the while continuing to visually monitor the client’s responses. The music therapist then begins to hum the melody of a chant used earlier in the session with lyrics about feeling grounded. The client responds by breathing deeply for a few moments without saying anything until their posture is more relaxed. The music therapist then fades the humming and provides the client with an opportunity to verbally process their associations to that song.
This vignette depicts a clinically-appropriate response to the client’s distress, which may have resulted in extended physical or psychological harm if not addressed immediately. The therapist practiced careful observation, recognized client-specific signs of distress, and verified the cause of distress with the client. Then, the therapist modified the other session components (i.e., the therapeutic application of a previous song referencing a practiced coping skill) to guide the client to a more comfortable state of arousal. In this example, the therapist’s strong intuition, vigilant observation, the client’s positive associations with the melody of the chant, and the client’s trust in the therapeutic relationship served as protective factors to mitigate harm.
Although these suggested steps can provide an immediate response to identified harm, professional supervision is a longer-term, more comprehensive solution to reducing harm on a broader level in music therapy practice. However, opportunities for mentored supervision are often sparse and not required after obtaining board-certification in the United States, despite AMTA Professional Competency C.19.1 recommending music therapists to participate in multiple forms of supervision. As such, the potential for negative effects and harm strongly implicate the need for more supervision for professionals, whether in informal peer settings, or formalized supervision relationships. Supervisory discussions regarding harm and reducing harm would expand and help normalize this topic, hopefully leading to a net reduction of harm among clinicians who engage in these conversations.
Educational and training implications in the United States
The MTHM also has clinical training implications for student music therapists as a potential educational tool for identifying specific sources of harm and protective factors against harm. Educational program standards for music therapists in the United States are guided by the AMTA Professional and Advanced Competencies (AMTA, 2013b, 2015). However, these two documents address harm-related topics differently and provide unclear expectations for how music therapy students of all levels should be taught about this crucial topic. Only the Advanced Competencies (AMTA, 2015) explicitly mention applying knowledge of contraindications in music therapy practice. Contraindications are not mentioned in the Professional Competencies (AMTA, 2013b) that govern entry-level practice. Instead, the Professional Competencies indirectly reference that clinicians “recognize and respond appropriately to situations in which there are clear and present dangers to the client and/or others” (AMTA,2013b, C.14.4). Thus, individual programs may not have clear guidance on how to prepare their students to meet the Scope of Practice’s (AMTA y CBMT, 2015) expectation that all music therapists incorporate knowledge of harm into their professional work.
The field of psychotherapy provides some initial insight into how educators may engage students in discussions regarding treatment and harm. Castonguay et al., (2010) suggested that educators raise awareness of potentially harmful therapies and critically examine with trainees the contextual factors that may produce harm. Additionally, these researchers suggested students be taught to observe and recognize when the therapeutic relationship is jeopardized in order to hone the experiential skills needed to repair problems in the therapeutic relationship. Although Castonguay et al., (2010) provided initial guidelines for psychotherapy students, the field of music therapy must contend with music and its resulting interactions with other session components as additional sources of harm. The MTHM may be incorporated into educational courses as a discussion framework for how negative effects may occur in practice. Such conversations between supervisors and trainees should not be one-time events, but instead a revisited discussion that evolves over a student’s training trajectory in practicum and internship. As a trainee’s clinical insight matures, supervisors should initiate and provide space for discussions about how harm may occur and be addressed.
Advocacy and legislative implications
A third major implication of the MTHM lies in the model’s potential to impact public perceptions of music therapy, along with related advocacy and legislative initiatives. In the past, music therapy has been presented as a therapeutic intervention that is noninvasive (Gardstrom, 2008) with few risks or side effects. This erroneous explanation of music therapy may diminish a lay person’s understanding of the unique and rigorous educational requirements of a board-certified music therapist. Although music therapists understand how their work differs from other music and health practitioners (e.g., therapeutic musicians, music volunteers), members of the public may blur or confuse the music therapist’s scope of practice with another music-health professional’s practice domain. By explaining a music therapist’s unique responsibility to assess, monitor, and respond to harm, the MTHM may further define and elevate the music therapy profession as one that requires specialized training and regulation. Furthermore, the MTHM provides a clear framework to articulate the potential for harm, with direct implications in the United States for AMTA and CBMT’s joint State Recognition Operational Plan (CBMT, n.d.). Currently, state task forces have few resources to explain exactly how proposed legislation to regulate music therapy practice would protect the consumers of music therapy. The MTHM may help task force members explain the concept of harm more clearly so that decision-makers (i.e., state legislators) can make informed decisions.
Research implications
The MTHM has several implications for future research in music therapy practice. The literature currently offers few insights into how harmful music therapy practices can be described, predicted, or explained. Furthermore, researchers do not consistently report negative effects or contraindications relevant to clinical practice. Incomplete reporting of harm is not limited to music therapy research. A review by Jonsson et al., (2014) of psychological treatment reporting found that only 21% of included studies indicated that signs of harm in patients were monitored and only 3% of reviewed studies provided a detailed overview of how harm was defined and measured. Healthcare disciplines continue to debate the best types of evidence for identifying negative effects, harm, and contraindications within therapy. Barlow (2010) posed several ideas regarding potential methods for discovering harm, including research design (e.g., randomized controlled trials versus case reports) and a timeline for monitoring harm (e.g., during active treatment versus a specific period after treatment ends). Additionally, Ioannidis et al., (2004) provided many helpful insights for reporting harm within randomized-controlled trials that may guide music intervention researchers.
Currently, Robb et al.’s (2010) guidelines for report of music-based interventions is the premier resource for best practices for communicating details of music-based interventions. However, these guidelines do not currently recommend reporting adverse, negative, or side effects of music-based treatments. Although institutional review boards provide oversight to protect study participants, researchers might consider having an explicit plan for monitoring and reporting the potential negative impact of a music-based intervention to ensure participant safety. If researchers consistently and transparently monitor negative clinical effects, then patterns relevant to understanding harm may begin to emerge. Additionally, collaboration with related music science disciplines may also bring to light the mechanisms underlying physical and psychological harm in music experiences so music therapists can more readily understand harm’s causes.
Global considerations
Finally, music therapy clinicians and educators should take special care when applying the MTHM in diverse global contexts. This writer’s music therapy education and career has been in the United States, and the MTHM’s development is inextricably linked to how music therapy is taught, practiced, and regulated in that country. The World Federation of Music Therapy lists 27 national music therapy associations as organizational members, spanning six continents (World Federation of Music Therapy, 2021). Within each association, music therapy exists in a unique dimension that includes the size of the field, the scope of the profession, and the degree to which clinical practice is regulated in that country. As such, music therapists in other countries should consider the cultural norms and regulatory standards of their country when framing and adapting the MTHM to their practice.
Summary and recommendations for future study
This paper presents a preliminary version of the Music Therapy and Harm Model (MTHM) for understanding the potential sources of physical or psychological harm within a music therapy session. Clinical anecdotes from both music therapists and clients suggest that this model may be helpful in organizing the field’s understanding of harm’s complexity. This model currently remains a theoretical framework in the absence of systematic research into this topic. Thus, the MTHM may continue to be refined via spirited discussion and ongoing study. The lack of scientific testing of the MTHM is a major limitation and the clinical and pedagogical suggestions made in this paper remain hypothetical in their effectiveness. As stated earlier, experimental research of harm in a clinical setting is a logistic and ethical challenge. Despite challenges in empirical testing into this paper’s propositions, several lines of inquiry may provide further insights.
First, a systemic review of literature is needed to gather information about currently known side effects, harmful effects, or contraindications of music therapy practice. This study would provide a foundation for what is currently understood about the negative effects of music interventions. Another potential study may gather and analyze observations of music’s negative effects as reported by board-certified music therapists, other practitioners implementing music-based interventions, or clients. Such a survey would also provide a starting point to understand the rate or types of adverse responses that may occur during TMEs. Additionally, creative research designs may find a way to ethically investigate how music can negatively impact human behavior, including gathering client reports of their experiences of music therapy’s negative effects. Future directions of research may then include the development of an assessment tool to systematically measure and collect data on how harm arises within clinical scenarios. Altogether, these efforts and a continued dialogue about harm within clinical music therapy practice will help differentiate music therapy from other music-health professions, raise clinical and training standards, and ultimately improve client outcomes.
Referencias
Abbot, E. (2005). Client experiences with the music in the Bonny Method of Guided Imagery and Music (BMGIM). Qualitative inquiries in music therapy, 2, 36-61.
Abrams, B. (2010). Evidence-based music therapy practice: An integral understanding. Journal of music therapy, 47(4), 351-379. https://doi.org/10.1093/jmt/47.4.351
Altenmüller, E., y Furuya, S. (2017). Apollos gift and curse: Making music as a model for adaptive and maladaptive plasticity. Neuroforum, 23(2), 57-75. https://doi.org/10.1515/nf 2016-A054
American Music Therapy Association (n.d.). Standards for education and clinical training. Retrieved January 20, 2020 from https://musictherapy.org/members/edctstan/
American Music Therapy Association (2013a). American music therapy association standards of clinical practice. Retrieved from https://musictherapy.org/about/standards/
American Music Therapy Association (2013b). American music therapy association professional competencies. Retrieved from https://musictherapy.org/about/competencies/
American Music Therapy Association (2015). American music therapy association advanced competencies. Retrieved from https://musictherapy.org/members/advancedcomp/
American Music Therapy Association (2019). Code of ethics. Retrieved from https://musictherapy.org/about/ethics
American Music Therapy Association, y The Certification Board for Music Therapists (2015). Scope of music therapy practice. https://musictherapy.org/about/scope_of_music_therapy_practice/
Barlow, D. H. (2010). Negative effects from psychological treatment. American psychologist, 65(1), 13-20. https://doi.org/10.1037/a0015643
Bronfenbrenner, U., y Morris, P. A. (2007). The bioecological model of development. Theoretical models of music development, 1. https://doi.org/10.1002/9780470147658.chpsy0114
Bruscia, K. E. (2014). Defining music therapy (3rd edition). Barcelona Publishers.
Carlson, E., Saarikallio, S., Toiviainen, P., Bogert, B., Kliuchko, M., y Brattico, E. (2015). Maladaptive and adaptive emotion regulation through music: A behavioral and neuroimaging study of males and females. Frontiers in human neuroscience, 9(466), 1-13. https://doi.org/10.3389/fnhum.2015.00466
Castonguay, L. G., Boswell, J. F., Constantino, M. J., Goldfried, M. R., y Hill, C. E. (2010). Training implications of harmful effects of psychological treatments. American psychologist, 65(1), 34-49. https://doi.org/10.1037/a0017330
Certification Board for Music Therapists (n.d.). Why state recognition of music therapy matters. Retrieved on January 20, 2020 from http://cbmt.org/advocacy/state-recognition/
Conroy, J. (2000). Unspeakable acts, ordinary people: The dynamics of torture. An examination of the practice of torture in three democracies. University of California Press.
Cusick, S. G. (2008). You are in a place that is out of this world…: Music in the detention camps of the “global war on terror.” Journal of the Society for American Music, 2(1), 1-26. https://doi.org/10.1017/S1752196308080012
Dimidjian, S., y Hollon, S. D. (2010). How would we know if psychotherapy were harmful? American Psychologist, 65(1), 21-33. https://doi.org/10.1037/a0017299
Edwards, J. (2011). A music and health perspective on music’s perceived “goodness”. Nordic Journal of Music Therapy, 20(1), 90-101. https://doi.org/10.1080/08098130903305085
Gardstrom, S. C. (2008). Music as a noninvasive treatment: Who says? Nordic Journal of Music Therapy, 17(2), 142-154. https://doi.org/10.1080/08098130809478205
Garrett, T., y Davis, J. D. (1998). The prevalence of sexual contact between British clinical psychologists and their patients. Clinical Psychology and Psychotherapy, 5, 253-263. https://doi.org/10.1002/(SICI)1099-0879(199812)5:4<253::AID-CPP171>3.0.CO;2-4
Garrido, S., Eerola, T., y McFerran, K. (2017). Group rumination: Social interactions around music in people with depression. Frontiers in psychology, 8(490). https://doi.org/10.3389/fpsyg.2017.00490
Gartrell, N. Herman, J. L., Olarte, S., Geldstein, M., y Localio, R. (1986). Psychiatrist-patient sexual contact: Results of a national survey. I: Prevalence. American Journal of Psychiatry, 143, 1126-1131. https://doi.org/10.1176/ajp.143.9.1126
Gattino, G. S. (2015). Some considerations about the negative effects of music. Musica Hodie, 15(2), 62-72.
Gutheil, T. G., y Brodsky, A. (2008). Preventing boundary violation in clinical practice. Gilford Press.
Hatfield, D., McCullough, L., Frantz, S. H. B., y Krieger, K. (2010). Do we know when our clients get worse? An investigation of therapists’ ability to detect negative client change. Clinical psychology and psychotherapy, 17, 25-32. https://doi.org/10.1002/cpp.656
Ioannidis, J. P., Evans, S. J., Gøtzsche, P. C., O’Neill, R. T., Altman, D. G., Schulz, K., y Moher, D. (2004). Better reporting of harms in randomized trials: An extension of the CONSORT statement. Annals of internal medicine, 141(10), 781-788. https:// doi: 10.7326/0003-4819-141-10-200411160-00009
Isenberg, C. (2012). Primum nil nocere (above all, do no harm): A direction for the development of music therapy. Canadian Journal of Music Therapy, 18(1), 62-78.
Jonsson, U., Alaie, I., Parling, T., y Arnberg, F. K. (2014). Reporting of harms in randomized controlled trials of psychological interventions for mental and behavioral disorders: A review of current practice. Contemporary clinical trials, 38, 1-8. https://doi.org/10.1016/j.cct.2014.02.005
Kalas, A. (2012). Joint attention responses of children with autism spectrum disorder to simple versus complex music. Journal of Music Therapy, 49(4), 430-452. https://doi.org/10.1093/jmt/49.4.430
Kaplan, P. W. (2003). Musicogenic epilepsy and epileptic music: A seizure’s song. Epilepsy y behavior, 4, 464-473. https://doi.org/10.1016/S1525-5050(03)00172-0
Lambert, M. J., y Barley, D. E. (2001). Research summary on the therapeutic relationship and psychotherapy outcome. Psychotherapy theory research y practice, 38,(4), 357-361. https://doi.org/10.1037/0033-3204.38.4.357
Leonard, H. (2020). A problematic conflation of justice and equality: The case for equity in music therapy. Music therapy perspectives, 38(2), 102-111. https://doi.org/10.1093/mtp/miaa012
Linden, M. (2013). How to define, find, and classify side effects in psychotherapy: From unwanted events to adverse treatment reactions. Clinical psychology and psychotherapy, 20(4), 286-296. https://doi.org/10.1002/cpp.1765
Linden, M., y Schermuly-Haupt, M. (2014). Definition, assessment and rate of psychotherapy side effects. World psychiatry, 13(3), 306-309. https://doi.org/10.1002/wps.20153
Loewy, J., Steward, K., Dassler, A. M., Telsey, A., y Homel, P. (2013). The effects of music therapy on vital signs, feeding, and sleep in premature infants. Pediatrics, 131((5), 902-918. https://doi.org/10.1542/peds.2012-1367
McCoy, A. (2006). A question of torture: CIA interrogation, from the Cold War to the war on terror. Metropolitan Books.
McFerran, K. S., y Saarikallio, S. (2014). Depending on music to feel better: Being conscious of responsibility when appropriating the power of music. The arts in psychotherapy, 41(1), 89-97. https://doi.org/10.1016/j.aip.2013.11.007
Murakami, B. (2018, March 1-4). A framework for understanding the potential for harm within music therapy [Conference presentation]. WRAMTA 2018 Conference, Ontario, CA, United States.
Murakami, B., y Goldschmidt, D. (2017, November 13-19). Music and harm: What we know and what we need to know [Conference presentation]. AMTA 2017 Conference, St. Louis, MO, United States.
Murakami, B., y Goldschmidt, D. (Hosts). (2018, October). Potential harm in music therapy? [Audio podcast]. https://amtapro.musictherapy.org/?p=2100
Nutt Williams, E. (2008). A psychotherapy researcher’s perspective on therapist self-awareness and self-focused attention after a decade of research. Psychotherapy research, 18(@), 139-146. https://doi.org/10.1080/10503300701691656
Otterman, M. (2007). American torture from the Cold War to Abu Gharaib and beyond. Melbourne University Press.
Pope, K. S., y Vasquez, M. J. T. (2007). Ethics in psychotherapy and counseling: A practical guide (3rd ed.). Jossey-Bass.
Proctor, G. (2002). The dynamics of power in counseling of psychotherapy: Ethics, politics, and practice. PCCS Books.
Rheker, J., Beisel, S., Kraling, S., y Rief, W. (2017). Rate and predictors of negative effects in psychotherapy in psychiatric and psychosomatic inpatients. Psychaitry research, 254, 143-150. https://doi.org/10.1016/j.psychres.2017.04.042
Robb, S. L., Carpenter, J. S., y Burns, D. S. (2010). Reporting guidelines for music-based interventions. Journal of Health Psychology, 16(2), 342-352. https://doi.org/10.1177/1359105310374781
Roskam, K. S. (1993). Cluttering the psychological house: The damage music can do. In Feeling the sound: The influence of music on behavior (pp. 49-61). San Francisco Press, Inc.
Rozental, A., Castonguay, L., Dimidjian, S., Lambert, M., Shafran, R., Andersson, G., y Carlbring, P. (2018). Negative effects in psychotherapy: Commentary and recommendations for future research and clinical practice. BJPsych Open, 4(4), 307-312. https://doi.org/10.1192/bjo.2018.42
Saarikallio, S., Gold, C., y McFerran, K. (2015). Development and validation of the Healthy-Unhealthy Music Scale. Child and adolescent mental health, 20(4), 210-217. https://doi.org/10.1111/camh.12109
Short, A. D. L., y Dingle, G. A. (2016). Music as an auditory cue for emotions and cravings in adults with substance use disorder. Psychology of music, 44(3), 559-573. https://doi.org/10.1177/0305735615577407
Standley, J. M., y Walworth, D. (2010). Music therapy with premature infants (2nd edition). The American Music Therapy Association, Inc.
Thaut, M. H., Thaut, C. P., y McIntosh, K. (2014). Melodic Intonation Therapy (MIT). In M. H. Thaut and V. Hoemberg (Eds.) Handbook of neurologic music therapy. Oxford University Press.
World Federation of Music Therapy. (2021, March 19). WFMT Membership. https://wfmt.info/wfmt-membership-2017-2020/
Yalom, I. D., y Leszcz, M. (2005). The theory and practice of group psychotherapy (5th ed.). Basic Books.

