Giant cell leiomyoma with red, hydropic and cystic degeneration: a case report
Leiomioma celular gigante con degeneración roja, hidrópica y quística: reporte de un caso
Gaceta Médica Boliviana, vol. 43, no. 2, 2020
Universidad Mayor de San Simón
Casos Clinicos
Received: 07 August 2020
Accepted: 04 November 2020

Abstract: Uterine myomas are fairly common neoplasms, classified according to their location in the myometrium: subserosal, intramural, transmural and submucosal. In turn, there are different morphological variants and degenerative changes that are a frequent phenomenon in myomas, especially the larger they are, such as apoplexy, atrophy, hyalinisation, red degeneration, cystic degeneration, peripheral calcification, necrosis, hydropic degeneration and malignant or sarcomatous degeneration. We report the case of a 53 year old female patient who underwent laparotomy where a tumour mass of 8150 grams was identified. The anatomopathological result was a giant leiomyoma with 3 different types of degeneration: red, hydropic and cystic. This case is reported due to the rarity of its conformation and the lack of reports in world literature. This is the first case presented and allows us to make some comments on the pathology.
Keywords: leiomyoma, uterus, benign neoplasm.
Resumen: Los miomas uterinos son neoplasias bastante comunes, se clasifican según su localización en el miometrio; subseroso, intramural, transmural y submucoso. A su vez existen diferentes variantes morfológicas y cambios degenerativos que son un fenómeno frecuente en los miomas, especialmente entre mayor tamaño tenga éste: como la apoplejía, atrofia, hialinización, degeneración roja, quística, calcificación periférica, necrosis, degeneración hidrópica y la degeneración maligna o sarcomatosa. Se expone el caso de una paciente de 53 años sometida a una laparotomía donde se identificó una masa tumoral de 8150 gramos, que dio como resultado anatomopatológico un leiomioma gigante con 3 diversos tipos de degeneración: roja, hidrópica y quística. Se informa este caso por la rareza en su conformación y debido a la falta de reportes en la literatura mundial, siendo este el primer caso presentando y permitiendo realizar algunos comentarios sobre la patología.
Palabras clave: leiomioma, útero, neoplasia benigna.
Uterine myomas are fairly common neoplasms and occur in 70% of women aged 45 years 1;.They are usually classified according to their location in the myometrium and can be subserosal (most common), intramural, transmural and submucosal (less common)1,2. Myomas sometimes occur in the broad ligament (intraligamentary), in the uterine tubes or in the cervix and because they respond to estrogen, they tend to enlarge during the reproductive years and decrease in size after menopause1.
There are different morphological variants of leiomyomas, from the point of view of the type, arrangement and appearance of the cellularity, number of mitoses and relation to the blood vessels involved according to the growth of the myomas (subirrigated)1,2,3. These alterations occur in 30% of cases and can appear at any age, but their maximum frequency is after the age of 40 years4.
There are also degenerative changes that are a frequent phenomenon in myomas, especially the larger ones3,5, such as apoplexy3;, atrophy that almost always begins after menopause and occasionally a little earlier4, hyalinisation (hyaline degeneration) which occurs in 60% of tumours and is the most common degenerative change which may involve areas or the whole tumor, assuming a homogeneous pale eosinophilic appearance, with blurring of the swirling pattern in areas of hyalinisation2,3,5. A particular form is red degeneration (usually appearing only during pregnancy and clinically manifested by acute abdominal pain)2,3,6: a myoma with red degeneration may in the long term develop peripheral calcification, most frequently in older women (menopause)4,5. Another rare form that a myoma can undergo is necrosis, which is seen on macroscopic examination as a pale grey, softened mass1,5; this occurs in approximately 10% of all cases, necrosis can occur in connection with menstruation, but most commonly during pregnancy and the postpartum period; it can also occur as a consequence of ingestion of ergot preparations4.
Hydrophilic degeneration is quite often observed in a focal form, sometimes this degeneration occurs diffusely within the myoma, which can result in different morphological patterns, such as: (a) perinodular hydropic change (b) hydropic change extending outside the confines of the leiomyoma resembling a myxoid leiomyosarcoma and (c) extensive or subtotal substitution of the leiomyoma by hydropic tissue accompanied by numerous vessels obscuring the myoid nature of the tumor; However, sometimes this type of change is very intense and can form cystic cavities, becoming a cystic degeneration that occurs in approximately 4% of uterine myomas 2,3. Finally, malignant or sarcomatous degeneration is very rare in only 0.29% of cases; this sarcomatous transformation begins in the centre of the tumour4.
All these alterations and variants of leiomyomas can sometimes cause confusion with the malignant counterpart of smooth muscle tumours, or with tumours of another histological type; the myomas most susceptible to this change are submucous myomas2,5
The case of a 53-year-old patient with a giant leiomyoma with 3 different types of degeneration is presented: being a rarity in its conformation and due to the lack of reports in the world literature, this being the first case presented and allowing us to make some comments on the pathology.
Case Presentation
A 53-year-old female patient was referred to the surgery department of the Cobija Clinic in the city of Cochabamba, Bolivia, presenting clinical symptoms of approximately 6 months’ duration, characterised by intermittent onset of abdominal pain that progressively increased, accompanied by abdominal distension and general malaise. She had no relevant past medical history.
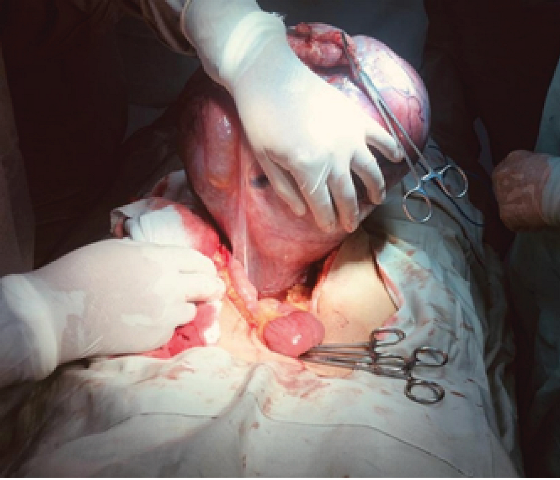
The patient is conscious, oriented, afebrile and normohydrated, with stable vital signs. The relevant findings on physical examination were: the abdomen was globular at the expense of the tumour mass, positive and normoactive hydro-aerial sounds, painful on superficial and deep palpation at the level of the hypogastrium (figure 1).

The patient was admitted with the diagnosis of a giant pelvic tumour; an ultrasound scan revealed a lesion occupying the abdominal cavity measuring 215*117 mm with a mixed ultrastructure.
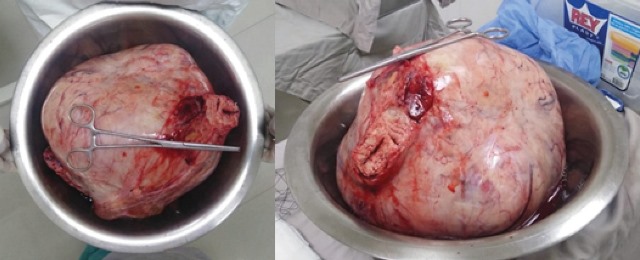
A laparotomy was performed with a supra-infrarumbilical midline incision, where the tumour mass was identified (figure 2), which was adhered to the uterus and adnexa, which led to its complete exeresis and subsequent incidental appendectomy, removing a total mass of approximately 9 kg, which was immediately referred for pathological examination (figure 3); the patient was discharged after 3 days without any complications.
Results
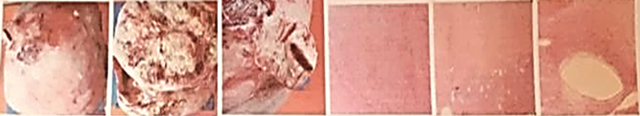
The anatomopathological study revealed a tumour of smooth and shiny external surface of 8150 grams, with a dimension of 29.4 * 18.6 cm, which was 80% solid and 20% cystic, the solid portion was firm, fasciculated and swirled, highlighting lax, myxoid and edematous areas; in its cystic portion the firm and smooth walls were occupied by a yellowish-green viscous material. Histologically, it presented diverse morphological variants such as areas of red degeneration characterised by coagulative necrosis, areas of hydropic degeneration due to accumulation of edematous liquid associated with collagen deposit with a filigree pattern and wide cystic areas resulting in a subserosal and intramural uterine fundus tumour compatible with cellular leiomyoma of diverse variants: red, hydropic and cystic degeneration (figure 4).
Discussion
Uterine leiomyomas are a worldwide health problem as they represent the most frequent reason for gynaecological consultations in our hospitals?. Uterine myomatosis affects 40% of women over 35 years of age. It is a benign neoplasm consisting of smooth muscle7, the following case report is classified as a large uterine leiomyoma, a term to be considered because of the rarity and clinical infrequency of these, terms that are manageable in medical-surgical practice when dealing with a case with such unusual proportions and dimensions. In most cases the myoma shows typical images, but degenerative changes can cause confusion in establishing the diagnosis9, as in our case given the morphology of the tumour.
In some cases the large size of the tumour mass does not allow the primary anatomical origin of the neoplasm to be correctly visualised by CT or other means8, the imaging technique for initial diagnosis is ultrasound, which is the least invasive and most cost-effective for patients9, in our case the ultrasound and CT imaging studies were useful for orienting the locations, but not for defining the exact site due to the size of the tumour.
CT is not very useful for delimiting myomas because it does not clearly differentiate myoma from normal myometrium, unless there are calcifications or necrosis9. Although the patient in our case had red degeneration, there were no areas of necrosis, so the CT scan was only useful for delimiting size.
Anatomopathologically, when the uterus was cut, we found that the myomas were hard, whitish with a pearly lustre. They may undergo cystic, hyaline, mucoid or myxomatous degeneration, fatty metamorphosis, calcification, red degeneration, septic necrosis and sarcomatous malignancy7. The classification of leiomyomas is based on growth pattern, histological appearance, association with blood vessels and eventually they may undergo degeneration3,8, as in the present case which went through red, hydropic and cystic degeneration.
In our case, this type of generation may lead us to think of another type of diagnosis such as a pelvic ovarian tumour, as in the case of Ortiz8 and Vega9, where the solid and cystic nature of the lesion led them to the presumptive diagnosis of a primary cystadenocarcinoma of the ovary8,9. But it was during the surgical procedure that it became evident that it came from the uterus, confirmed by the anatomopathological study, a case similar to the one mentioned by Ortiz et al 8.
The atypical clinical presentation of degenerated uterine leiomyoma can lead to misdiagnosis; case reports of leiomyomas with extensive cystic degeneration, simulating ovarian cystadenocarcinoma are rare8. Because of the macroscopic appearance of this benign tumour it is important to take it into account in the intraoperative study: thus determining the most appropriate surgical approach for each patient and extensive sampling of the surgical specimen10,11.
In conclusion, the surgeon must keep giant leiomyoma in mind in the differential diagnosis of malignant epithelial neoplasms of the ovary8and it is therefore important that the pathologist and treating physician take into account this morphological variant (size and degeneration) to avoid confusing it with other entities with the consequent error in therapeutic management3.
Dedication
To our dear teacher and colleague “Doctor Gilberto Ferrufino Navia” who will live for eternity and one more day in our memories, whom neither fatigue nor adversity could defeat.
References
1. Hernández VM, Valerio CE, Tercero VCL, Barrón VJ, Luna RRM. Miomatosis uterina: implicaciones en salud reproductiva. Ginecol Obstet Mex. 2017 septiembre;85(9):611-633. Fecha de acceso: 20/02/2010. Disponible en: www.ginecologiayobstetricia.org.mx [ Links ]
2. Ruiz CL, Hernández AM, Villalobos SFJ, Abad RC, Parra CMA, Ramón JM y Cajal, Vela LA. Caso de un leiomioma quístico gigante que simula una tumoración ovárica. Progresos de obstetricia y ginecología. Disponible online el 3 de octubre de 2015 Fecha de acceso: 18/02/2010. Disponible en: https://www.elsevier.es/es-revista-progresos-obstetricia-ginecologia-151-avance-resumen-caso-un-leiomioma-quistico-gigante-S0304501315001880
3. Luévano FE, Aldrete TJ. Leiomioma con degeneración hidrópica perinodular. Reporte de un caso II congreso virtual de anatomía patológica Fecha de acceso: 18/02/2010. Disponible http://www.conganat.org/iicongreso/posters/008/intro.htm
4. Tumores ginecológicos benignos. Revisión bibliográfica Ginecología y Obstetricia 25 mayo, 2013. Fecha de acceso: 24/02/2010. Disponible en https://www.revista-portalesmedicos.com/revista-medica/tumores-ginecologicos-benignos-revision-bibliografica/5/ [ Links ]
5. Ortiz RME, Matute LA, Martínez CN. Miomatosis uterina. ANALES MEDICOS Vol. 54, Núm. 4 Oct. - Dic. 2009 pp. 222 – 233. Fecha de acceso: 18/02/2010. Disponible en: www.medigraphic.com? pdfs ? abc
6. Tomás Pérez-Luco A. Patología benigna y maligna de utero. Sintensis biblioteca digitaldinamica para estudiantes y profesionales de la salud. Fecha de acceso: 20/02/2010. Disponible en https://sintesis.med.uchile.cl/index.php/respecialidades/r-ginecologia-y-obstetricia?id=1647 [ Links ]
7. Vargas HV, Vargas AVM, Tovar RJM, Flores BK, Acosta AG, Moreno EMA. Leiomiomatosis uterina. Aspectos epidemiológicos, fisiopatogénicos, reproductivos, clínicos y terapéuticos. Rev Hosp Jua Mex 2013; 80(3): 173-182. Fecha de acceso: 24/02/2010. Disponible en www.medigraphic.com ? pdfs ? juarez [ Links ]
8. Ortiz GJ, Puente PL, Uscanga CE, Espinoza ME, Coronel BPG. LEIOMIOMA QUÍSTICO GIGANTE QUE SIMULA UN CÁNCER DE OVARIO. INFORME DE UN CASO. REVISTA SALUD QUINTANA ROO. Fecha de acceso: 24/02/2010. Disponible en https://salud.qroo.gob.mx/revista/revistas/23/4.pdf
9. Vega-RFJ, Barceló-MDA , Gutiérrez-de la Vega, Luis-ZH. Leiomioma quístico gigante que simula una tumoración ovárica. Reporte de un caso. Ginecol obstet. Méx. vol.85 no.5 Ciudad de México may. 2017. Fecha de acceso: 24/02/2010. Disponible en http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0300-90412017000500325
10. Ibáñez, MIM, Ríos MJ, Pascual LM, Fuertes ZA, Valero PI, Gimeno EE. Leiomioma cotiledonoide disecante del útero.A propósito de dos casos y revisión de la literatura. REV ESP PATOL 2005; Vol 38, n.º 4: 243-246. . Fecha de acceso: 24/02/2010.
11. Moyano Crespo G, Manrique V, Ramat M, Maldonado F, Suarez Ghibaudo MH, Volmaro K, Herrero MV, Matsuzaki M. LEIOMIOMA CON CAMBIOS HIDRÓPICOS Y DEGENERACIÓN QUÍSTICA (TIPO LEIOMIOMA DISECANTE COTILENOIDEO. Revista de la Facultad de Ciencias Médicas 2016; Supl.(1). . Fecha de acceso: 24/02/2010. Disponible en webs.fcm.unc.edu.ar › articulos › Clinica.quirurgica [ Links ]

