Abstract: 4. Govindarajulu Arun Prasad MD, F.R.C.A., DA, Anahi Perlas, M.D., F.R.C.P.C., Ki Jinn, M.D., F.R.C.P.C., Vincent Chan, M.D., F.R.C.P.C. Ultrasound Assisted Spinal Anesthesia in Morbidly Obese Patients. 2008; A339:1. Available from: http://www.asas.com/strands/asas/.htm?absnum=1486&index=17&year=2008. 15. R R-M. Opciones de abordaje neuroaxial. Acceso de Taylor. 2016; 39: S182-S4. Available from: https://www.medigraphic.com/pdfs/rma/cma-2016/cmas161bj.pdf. [ Links ]
Keywords: anesthesia, lumbar, ultrasound.
Resumen: La ecografía es una herramienta de gran ayuda en medicina, rápido, tecnología portátil y segura. Así por ejemplo realización de la punción lumbar (accesos vasculares y bloqueos regionales) para la obtención de líquido cefalorraquídeo por médicos de emergencia y anestesiólogos, etc. Como ventajas tenemos: disminución del número de punciones lumbares, satisfacción del paciente. Es una alternativa en pacientes con alta probabilidad de punción lumbar difícil como por ejemplo: pacientes obesos, pacientes con edema, con antecedentes de cirugía columna previa, escoliosis. En el presente artículo tiene como objetivo brindar información sobre la utilidad de la ecografía en la punción lumbar en adultos y la obtención del líquido cefalorraquídeo. Proponer una abordaje metódico para puncion lumbar y el bloqueo neuroaxial en tiempo estático por ecografía de la columna lumbar del adulto. Se realizó la búsqueda de la bibliografía de revistas académicas de medicina y anestesiología disponibles en base de datos confiables.
Palabras clave: anestesia, lumbar, ecografia.
Articulos de Revision
Use of static time ultrasound for lumbar puncture
Received: 01 October 2020
Accepted: 01 December 2020

The use of ultrasound was first performed as a puncture according to the Russian literature in 1971 were the neuroaxial anatomy was delineated, being identified as e.g. structures of the lamina, yellow ligament, spinal canal and vertebral body. As well as measuring the lamina space and the epidural space before the epidural procedure1,2.
On the other hand, this kind of usefulness and access through ultrasound is not only limited to anaesthesiologists, but also to medical health personnel for obtaining cerebrospinal fluid samples such as emergency physicians, internists and intensive care physicians.
Ultrasound is limited by some aspects which could be the skill of the person performing it, type of ultrasound machine, types of patients and interferences in the image. But even so, ultrasound is one more method that would contribute to obtaining an image that is only possible through the inter-laminar spaces between adjacent vertebrae where it would allow sound waves to enter the vertebral canal and thus also enter the space with the spinal needle1.
The type of information search for this review topic is of explanatory content, searching primary and secondary sources, recognised scientific journals and databases. Articles related to the use of ultrasound for neuroaxial anaesthesia in adult patients were selected. The validity of these articles is that they meet the international criteria for the publication of scientific studies, such as the uniformity requirements of the International Committee of Medical Journal Editors.
The aim of this work was to carry out a descriptive review of the literature to provide information on the usefulness of ultrasound in lumbar puncture in adults, the collection of cerebrospinal fluid and the procedure for spinal anaesthesia. To propose a methodical approach for neuraxial blockade in static time by ultrasound of the adult lumbar spine.
Methodology
A bibliographic search was carried out in October 2020 in databases of scientific journals, using the descriptors: ultrasound and neuraxial anaesthesia, review articles, original articles, abstracts of articles in preparation and short publications. We obtained 20 out of 117 records after combining the keywords in “Anesthesiology”, an internationally recognised North American journal. In addition, an internet search was carried out in the search engine “google academic” with similar terms. The selection criteria for the articles were: use of ultrasound in neuraxial anaesthesia, spinal anaesthesia, procedures to perform ultrasound-guided neuraxial blockade in adult patients.
Desarrollo
Anatomy of the spine: Typically, the vertebra is made up of a body and an arch. The latter would have the following parts: pedicle, lamina, spinous processes and superior and inferior articular processes. Thus some terms have to be understood as “interlaminar space” synonymous with the adjacent laminae and “interspinous space” synonymous with spinous processes in the description of this paper.
It was noted that the only acoustic windows to look for are: intervertebral foramina (lateral) and inter-laminar spaces (posterior). Ligamentum flavum (yellow ligament) is the ligament that joins the inter-laminar spaces, this ligament has a superficial and deep component. And the spinous processes joined by the interspinous ligament. The vertebral canal which is formed by thecal sac itself containing dura mater and arachnoid.
The ligamentum flavum has been recognised sonographically since 1995 and may be helpful in identifying and accessing the epidural space. Accompanied by the use of a curved transducer with low frequencies of 4-7 MHz3.
It also consists of five lumbar vertebrae having an anterosuperior direction, and thoracic vertebrae having broad, flat, almost vertical spinous processes.
The conus medullaris generally in the adult is located at L1, first lumbar, and the thecal sac ends at the level of the first sacral S11.
On the other hand, understanding some aspects, principles of ultrasound is important such as: the types of transducers and their uses will avoid using the wrong one for the different structures to be inspected, ultrasound terms such as: anechoic which is represented in black colour indicates a structure that does not generate echoes, hypoechoic in grey colour which indicates that it generates echoes of little or low intensity. And hyperechoic of bright white colour which generates echoes of great intensity. Types of cut that can be transversal, sagittal, etc4.
Image orientation is related to one side of the screen, as if you were looking at the patient from the front5.
Indications for the use of spinal neuraxial ultrasound. The development of this skill or competence in healthcare personnel, and now for the anaesthesiologist, implies a commitment to continuous education, with the aim of providing a better quality of patient care and thus avoiding patient complications. It would be indicated in those spines that are likely to be difficult to puncture, taking into account the following variables: age, non-palpable landmarks (obesity, oedema), personal history of previous spinal surgery, or deforming spine such as ankylosing spondylitis, scoliosis. A score of four points or more would predict a difficult puncture6,7.
Orderly approach technique for static time ultrasound blockade of the adult lumbar spine for spinal neuraxial anaesthesia.
Scoring and patient assessment for possible predictors of lumbar puncture difficulty..
1. The patient will be given an explanation of the procedure to be performed prior to surgery, as well as the use of ultrasound, which will be described as follows1: preparation for the examination, the patient will be positioned for the bagging procedure, which may be performed in a sitting or lateral dorsal decubitus position.
The use of a low frequency curved transducer (2-5 MHz) is recommended. The high-frequency transducer or linear transducer (10-12 Mhz) can also be used, which provides a rectangular image on the monitor, has low penetrance (2-4cm) but with high image resolution; consider this transducer in thin patients. The ultrasound machine should be adjusted: generally 7-10cm, focus and gain adjustment on the ultrasound machine as necessary. Some aspects should not be neglected such as: reducing the beam frequency, adequate pressure of the transducer on the skin that has a good contact and compresses the overlying tissue. Have ready the number 22 needle or larger with lengths greater than 90 mm. Or Braun-Germany 25 G B needle, pencil point needle.
The transducer should be protected with an insulator prior to gel placement. Another option would be to perform the marking with a demographic marker, then carefully remove the gel material from the skin, the marking on the skin will be with an indelible marker, it is important to properly remove the gel remains from the skin of the puncture site because it is not known what complications it could cause, if this gel enters the spinal space. Some suggest replacing the gel with physiological saline to avoid this event7.
A complete aseptic technique with gloves, gown, mask and sterile equipment should be in place. Sterile equipment for the lumbar puncture should also be ready.
Consider sedation of the patient according to the patient’s characteristics, although it will only be the marking with ultrasound, not a real-time puncture with the transducer. The latter has a different description and is also performed by experienced anaesthesiologists. The patient will be offered oxygen administration with a mask.
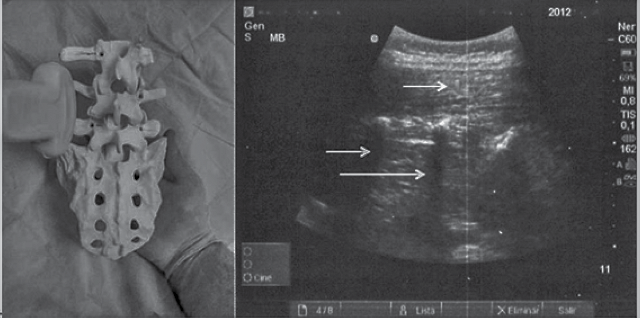
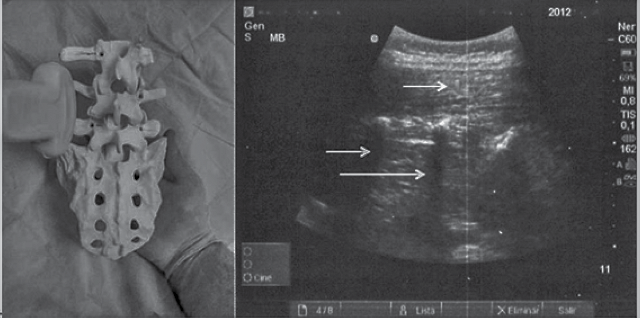
2. Proceed to the anatomical examination with the aid of the ultrasound scanner. Observe the sagittal median transverse process, place the transducer probe in the sagittal paramedian 3 - 4 cm from the midline. Then the “trident sign” will be observed being represented by the finger-like acoustic shadows of the transverse processes. At the level of L2-L3 this sign is observed. Remember that the lumbar plexus lies more than 2 cm below the transverse process8,9(Figure 1).
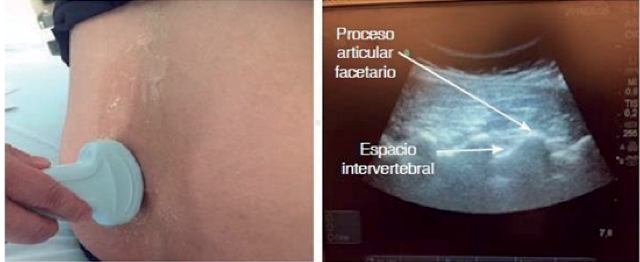
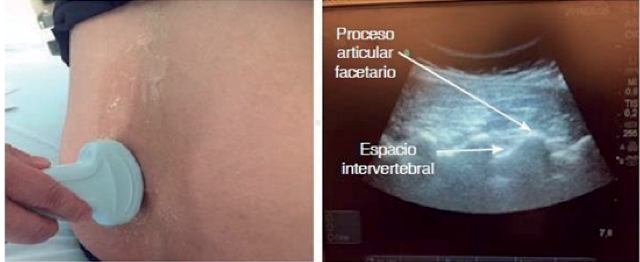
3. Observe from the sagittal paramedian articular process. Place the probe medially towards the midline maintaining an orientation, obtaining the image of rounded “humps” of the facet joints between the superior and inferior articular processes (Figure 2).
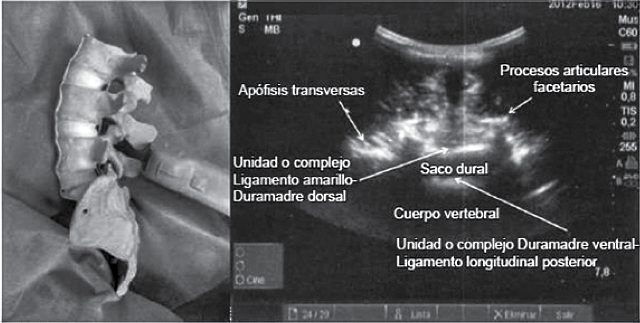
4. Observe with sagittal paramedian oblique view, look for the image of the sagittal paramedian articular process, tilt the probe towards the midline to obtain the sagittal paramedian oblique view. Additional small sliding and tilting movements of the probe may be required to optimise the view. We will obtain a “saw-tooth” appearance of the laminae. At the level of L2-S1 such an image is seen, so seeing the posterior longitudinal ligament (PLL) would qualify as a good image if it were bright (it may also be absent or hazy), the absence of this ultrasound image is a predictor of difficult spinal puncture10(Figure 3).
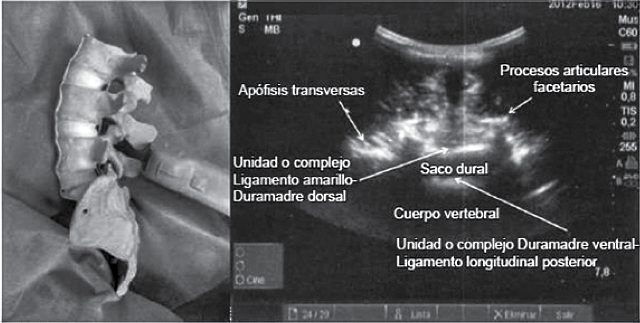
Posterior complex (yellow ligament, epidural space and posterior dura mater). Anterior complex (anterior dura, posterior longitudinal ligament, vertebral body)9.
For the vertebral count, first identify the sacrum, which is observed ultrasonographically by placing the transducer over the sacrum 2-3 cm to the right of the midline in order to visualise the hyperechogenic line corresponding to the sacrum. Move in the cephalic direction to obtain the aforementioned “saw” image, “fisted knuckles” which are the articular processes and can reach L3-L411.
Perform slow cephalic to caudal movement until absence of acoustic shadow is obtained. Sometimes it is not possible to identify the image of the yellow ligament complex and the dura mater as two structures. We may only observe a single hyperechogenic line, then mark with a demographic pen corresponding to the puncture site12.
5. Identify and mark the intervertebral levels: slide the probe in caudal movements maintaining an oblique Paramedian Sagittal Sagittal orientation, until the L5-S1 intervertebral space is centred on the Ultrasound screen, its location will correspond to the midpoint of the long side of the probe and may be marked on the patient’s skin.
The probe shall then be moved in a cephalad direction, centring each successive intervertebral space (L4-L5, L3-L4, L2-L3) on the ultrasound screen AND marking it on the patient’s skin (“progressive counting” method from the sacral portion upwards). The identity of the intervertebral spaces can be confirmed by identifying the T12 vertebra by its articulation with the 20th rib and then sliding the probe in a caudal direction to visualise each successive intervertebral space (the “countdown” approach). It is important to identify the hyperechoic horizontal line of the sacrum. The 20th rib and its articulation with the transverse process of the T12 vertebra.
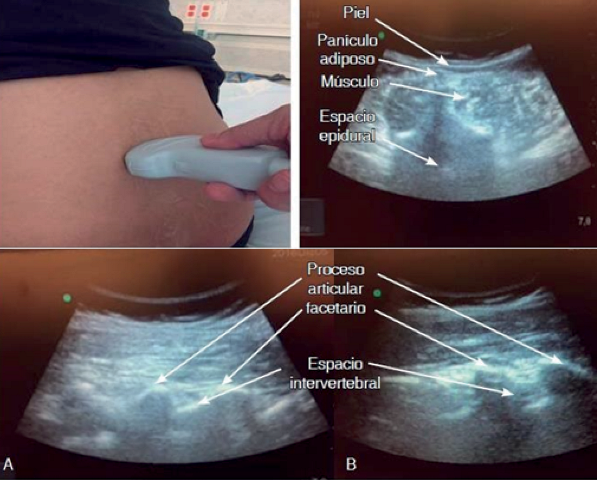
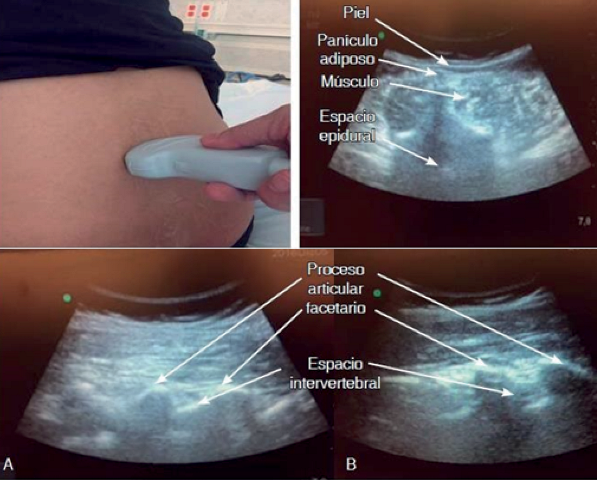
6.- Interlaminar Transverse View: Rotate the probe 90 degrees in a transverse orientation and slide it cephalad or caudally as necessary to obtain interlaminar transverse views of the desired interspaces (L2-L3, L3-L4, L4-L5). It is permissible for the probe to be tilted cephalad to optimise the view.
Calculate the required depth of needle insertion by measuring the depth from the skin to the posterior complex using the electronic calipers on the Ultrasound machine it is now essential to see the articular process of the interspinous ligament and transverse process anterior complex posterior complex.
The measurement will be performed with the measuring button or caliper of the ultrasound scanner which is integrated in the button panel. Its function will be important as it helps us to measure the proportions of the structures we are studying or the velocities of the blood in vascular studies. Or the caliper may also be located on the screen. We then measure the distance from the skin to the anterior portion of the yellow ligament-duramadre complex, which will be the lower limit of the intrathecal depth or an approximation of the depth of the epidural space12,9. This would be a measurement of the epidural space. This would be an indirect measurement of the intrathecal space or depth. This in the transverse plane or approach and the longitudinal paramedian as a complementary tool (Figure 4).
7. The needle insertion point for a midline approach should now be marked: centre the neuraxial midline on the ultrasound screen. In the transverse interlaminar view and mark the midpoint of the long and short sides of the probe. The intersection of these two marks indicates the point of needle insertion. Perform spinal or epidural anaesthesia in the usual manner, guided by the skin markings and depth measurements. Needle redirections, if necessary, are usually small and in a cephalad direction.
Some considerations in patients with predictors of difficult lumbar puncture such as: in elderly patients the interspinous and interlaminar spaces are narrow. This makes imaging difficult, so with a transverse view of the vertebral canal it may be difficult to visualise, so a sagittal paramedian oblique view would be a good option. The previous marking in these patients due to their flaccid and mobile skin can vary the puncture. In order to solve this mobility of the skin, it could be convenient to have the help of a person to keep the skin firm where the marking was initially made.
The literature mentions that the interspinous and interlaminar space at the L5-S1 level is the most easily located on ultrasound and is therefore useful in the elderly13.
In obese patients, identify and obtain a parasagittal view of the sacrum, then move the probe cephalad to identify the lumbar vertebral laminae from L5 to L1. When at the L3-L4 level, the probe should be rotated 90° degrees to obtain a transverse view, the spinous process space to identify the Flavo or dura complex along the midline. Then mark on the skin this reference14,9. Or in the pregnant woman with fluid retention, if it is difficult to visualise, the following could be performed as pressure on the transducer to compress the subcutaneous structures. Although the estimated distance will vary a little, it will help you to better visualise.
Now a patient with spinal surgery may be imaging or visualising the metalwork if there is a pathway to perform the neuraxial block6.
The use of ultrasound is being applied in various areas of medicine, so this review topic describes the information according to our objective, which is to provide information on the use of ultrasound to identify the lumbar space, having this data allows us to have access to obtaining the lumbar puncture in the field of Anaesthesiology, we can provide the patient with a spinal neuraxial anaesthesia. Studies have shown that it improves the quality of patient care and the degree of patient satisfaction, because it requires fewer needle manipulations for success and the time needed for the block.
At the same time it reduces possible complications such as: if peridural puncture is performed, it avoids inadvertent puncture of the dura mater, vascular puncture and paraesthesia. The latter were reduced by up to fifty percent1.
It can also be used to predict difficult lumbar puncture, including the following criteria: presence of deformity, obesity (body mass index greater than 33 kg/m2), history of difficult lumbar puncture, spinal surgery, absence of palpation landmarks, patients with oedema in the region to be punctured 1.
Also these patients with predictors of difficult lumbar puncture could make it difficult to obtain the ultrasound image, providing poor quality images. For example, in obese patients, the structures are attenuated, which occurs when the waves travel at a greater distance from the soft tissues15. A possible help to solve this difficulty with the help of ultrasound technology could be to use harmonic ultrasound imaging.
It has been observed in some studies that in order to acquire this competence in the use of ultrasound for spinal puncture, it is necessary to have an average of 40 patients in practice to acquire this skill or competence1.
Most of the studies to evaluate the measurement of depth by ultrasound are for epidural anaesthesia, with the measurements found in 300 patients being an average depth of 51.2 +/- 7 mm Graul et al. in epidural anaesthesia and another study carried out in 100 patients with a depth of 53+/-7mm Grul et al.12, so it would be advisable in the not too distant future to carry out more studies to make comparisons.
We can conclude that the use of ultrasound is important as a very useful tool for the benefit of the patient. Thus, all physicians should be trained in its appropriate use when required, and we anaesthesiologists are not exempt, we should acquire this competence. The literature suggests that basic knowledge of ultrasound should be recognised first, and it is also recommended that this ability or competence should be cultivated from the first years of study in residency, so that in the future we can have greater expertise in this broad field of ultrasound.
Practice with patients with normal spinal anatomy and then progress to patients with predictors of difficult lumbar puncture.
The lack of practice with ultrasound is due to the limited access to a sophisticated bedside ultrasound scanner in the performance department. This makes it difficult to recognise the spinal anatomy ultrasonographically in order to develop interventional skills.
However, with the experience gained, the real-time ultrasound-guided neuraxial anaesthesia procedure could be performed, but it also requires a trained person to assist you in the procedure.
So the use of static time ultrasound for spinal anaesthesia helps to provide quality anaesthesia because there is an increase in patient satisfaction, fewer attempts to perform spinal anaesthesia, improved patient safety.