Prothrombin time and activated partial thromboplastin time usefulness in the preoperative assessment of hemostasis in pediatrics.
Gaceta Médica Boliviana, vol. 43, no. 2, 2020
Universidad Mayor de San Simón
Articulos Originales
Received: 24 August 2020
Accepted: 31 October 2020

Abstract:
In order to evaluate hemostasis preoperatively, clinical history and physical examination are required, and the use of coagulation tests is recommended only when there is an indication, and not as a routine procedure.
Objetive: the present study aims to determine the usefulness of TP and APTT in the preoperative assessment of coagulopathies in scheduled minor and outpatient surgeries.
Methods: we conducted a prospective, observational study in a tertiary surgical hospital; we selected patients undergoing minor and ambulatory procedures, excluding those with comorbidities, high surgical bleeding risk or with medication that interferes with coagulation.
Results: 69 patients were recruited, clinical history and directed physical examination were applied identifying 1 patient suspected of coagulation disorder (later discarded); 218 complementary examinations were performed: 69 routine (TP, APTT, hemogram) and 149 non-routine (arbitrarily indicated), obtaining mean values in normal ranges and not being able to identify or rule out coagulation disorders with them, but observing 21% (15 cases) abnormal results, which additionally caused behaviors to confirm or correct these values, ranging from repeating the test to transfusing hemoderivatives; generating an overall average cost of 102 Bs. 102 Bs. per patient, without benefit or change in clinical or surgical conduct.
Conclusion: the study established that routine preoperative screening tests are of little use and are not very cost-effective in the evaluation of hemostasis for minor or ambulatory procedures, compared to a clinical history and directed physical examination; their indication is appropriate when there are abnormal findings in the physical examination and clinical history or based on concomitant diseases.
Keywords: screening, hemostasia, pediatric surgery, preoperative assesment.
Resumen:
Para evaluar la hemostasia preoperatoriamente una historia clínica y examen físico dirigidos están indicados, siendo el uso de pruebas de coagulación recomendados solo cuando existe alguna indicación, y no de rutina;
Objectivo: el presente estudio pretende conocer la utilidad del TP y APTT en la valoración preoperatorio de coagulopatías en cirugías programadas menores y ambulatorias.
Métodos: se realizó un estudio prospectivo, observacional en un hospital quirúrgico terciario; seleccionamos pacientes sometidos a procedimientos menores y ambulatorio, excluyendo aquellos con comorbilidades, riesgo quirúrgico de sangrado alto o con medicación que interfiera con la coagulación.
Resultados: se reclutaron 69 pacientes, se aplicó la historia clínica y el examen físico dirigido identificando 1 paciente sospechoso de trastorno de coagulación (posteriormente descartado); Se realizaron 218 exámenes complementarios: 69 rutinarios (TP, APTT, hemograma) y 149 no rutinarios (Indicados de forma arbitraria), obteniendo valores medios en rangos normales y no pudiendo identificar o descartar trastornos de coagulación con ellos, pero observando un 21% (15 casos) resultados anormales, lo que adicionalmente ocasiono conductas para confirmar o corregir estos valores, que van desde repetir la prueba a transfundir hemoderivados; generando un costo promedio global de 102 Bs. por paciente, sin un beneficio o cambio en la conducta clínica o quirúrgica.
Conclusion: el estudio estableció que las pruebas rutinarias de screening preoperatorio tienen poca utilidad y son poco costo-beneficiosas en la valoración de la hemostasia para procedimientos menores o ambulatorios, en comparación de una historia clínica y examen físico dirigido; siendo apropiada su indicación cuando existan hallazgos anormales en el examen físico e historia clínica o en base a enfermedades concomitantes.
Palabras clave: screening, hemostasia, cirugía pediátrica, valoración preoperatoria.
Surgical pathology in pediatrics represents a frequent cause of care in daily practice. It is currently accepted, when scheduling minor surgery or an outpatient procedure, to request complementary tests to screen for coagulation disorders only in cases where a family history of coagulopathy or a clinical history and physical examination suggestive of a coagulation disorder is identified, or if genetic information on the biological family is not evaluable1-3. The level of evidence supporting these recommendations is based on observational studies, but not on randomized clinical trials, which generates controversy when applying these recommendations, especially in establishments with limited resources and in populations with a high prevalence of anemia and malnutrition, which could have repercussions and in some way differ from the population studied in the aforementioned studies4-15. Knowing these data will provide useful information at the time of pediatric preoperative evaluation and will allow cost/benefit decisions to be made for the patients and the institution.
The aim of this study was to determine the usefulness of TP and APTT in preoperative screening for coagulopathies in children undergoing ambulatory surgery or minor programmed operations in the Department of Surgery of the Hospital del Niño Manuel Ascencio Villarroel (HNMAV).
Material and methods
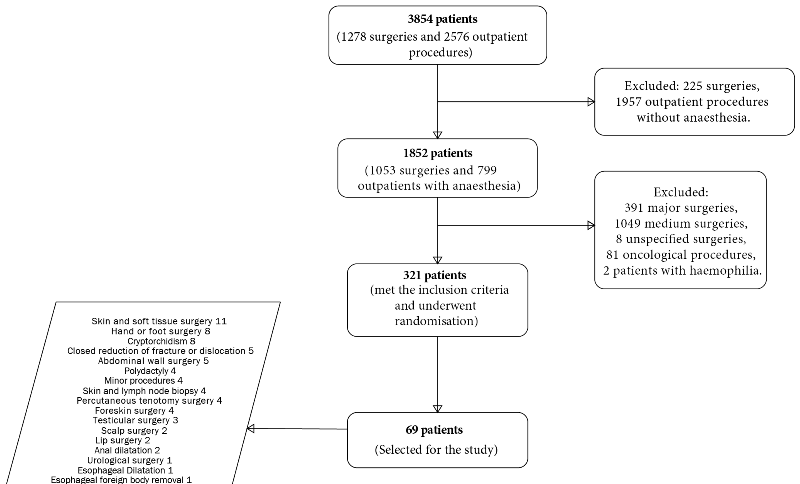
A single-center, prospective, observational study was designed in the pediatric surgery area of the HNMAV, the only public sector hospital of 3rd level of complexity with this service, a sample size of 69 patients was established, considering a margin of error of 5%, and 95% confidence for a finite universe of 321 minor and scheduled surgeries; they were recruited from January 2019 to completion of the sample in June 2020. Patients without previous comorbidities (known hepatic, hematologic, oncologic or nutritional), with outpatient procedures or minor surgeries, low estimated bleeding risk, without medication that interferes with coagulation, were included in the study.
Data collections were performed in two times:
Time 1: During the preoperative outpatient pediatric evaluation or on the first day of hospitalization, the following measurements were performed:
Completion of the questionnaire suggested by Rapapport1 Searching and recording of clinical findings suggested by Chee2. Request and recording of TP, APTT and platelet test results and others suggested by the attending surgeon or the anesthesiology team.
Time 2: Early and late postoperative period.
Record of early (hours) and late (days) bleeding complications after surgery. Recording of laboratory costs, medication and hemoderivates consumed by the patient to correct coagulogram alterations.
The data was analyzed with the IBM statisttics SPSS v25 program, performing descriptive statistics of central tendency and a bivariate analysis of linear correlation between the variables studied and the results (hospital outcomes and costs).
The study was approved by the bioethics committee of the HNMAV in October 2018, being a descriptive study without human intervention, the use of a specific informed consent was obviated, all ethical considerations suggested by the committee were kept in mind.
Results
The study enrolled a total of 69 patients who met the inclusion and exclusion criteria for the study, showing a variety of different ambulatory and minor surgical procedures within the sample (Graph1).
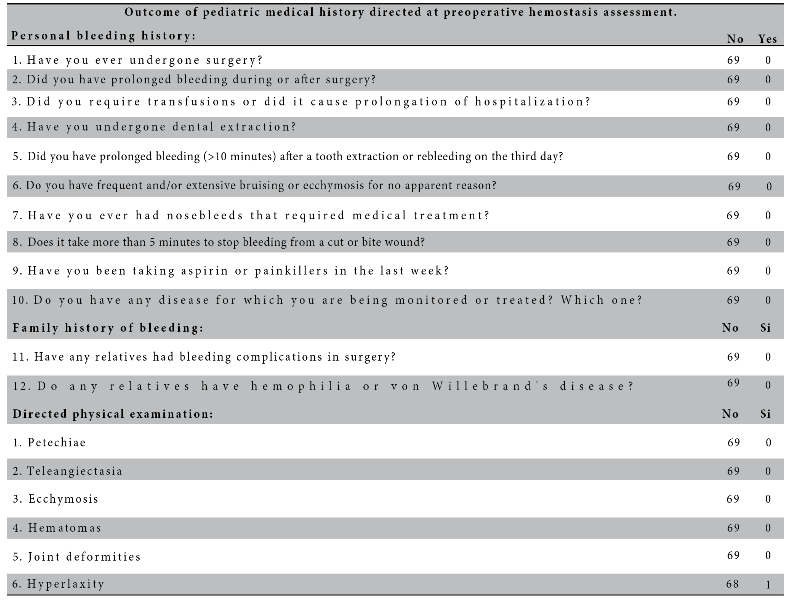
In 69 patients 218 complementary examinations were performed (69 routinely and 149 non-routinely), in the cases in which non-routine examinations were requested the most frequently required were creatinine 47.8%, urea 36.2%, glycemia 26.1% Na and K 17%, Cl and Ca 14.5%, GOT and GPT 11.5%, coagulation time 18.8% and bleeding time 2.9%; The reason for these requests is based mainly on the criteria of the treating surgeon or the anesthesiologist who will assist in the procedure, it is worth mentioning that no patient has known comorbidities or underlying pathology in the clinical history and that only in one case was there evidence of a finding suggestive of coagulopathy on physical examination, the other patients having no pediatric indication that clinically justifies the request for these studies. The results of the tests requested in terms of mean values and standard deviation were within normal ranges for age (Table 2).
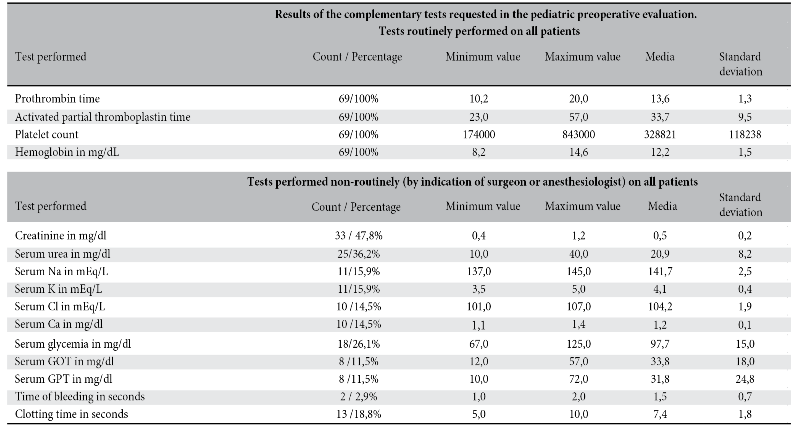
As for the benefits of applying the clinical history aimed at assessing hemostasis, it was found to be useful in detecting patients suspected of having problems in hemostasis in 1.5% of the cases; however, the use of screening by requesting complementary tests did not allow identifying or ruling out cases of coagulation disorders, although in 21% (15 cases) the results, mainly of TP, were altered (false positives), which additionally caused to engage in actions to confirm or correct the altered results, resulting in 4 main conducts, 1: repeat the altered studies 4 cases (6%), 2: repeat the altered studies and administer vitamin K 3 cases (4%), 3: administer vitamin K 7 cases (7%), 4: transfuse Fresh Frozen Plasma 3 cases (4%) (Table 3).
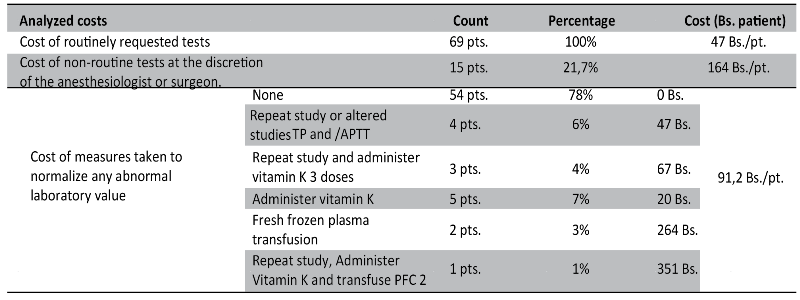
As for the costs generated by the performance of routine examinations in patients undergoing minor or outpatient procedures, we found an average cost of 47 Bs. per patient, an average additional cost of 164 Bs. for non-routine examinations and 91 Bs. for corrective or confirmatory measures in the event of altered results; with an overall average cost of 102 Bs. per patient undergoing minor or outpatient surgical procedures (Table 3).
Discussion
In daily practice, it is still widely accepted to request blood tests for hemostasis screening in children undergoing minor or ambulatory surgery,10,14 although their utility is low diagnosing severe coagulopathies or predicting perioperative bleeding in healthy children; on the other hand, their value is unquestionable in patients with anticoagulation, or in patients with known preoperative coagulation factor deficiencies.
The clinical findings and the physical examination aimed at assessing hemostasis identified only one patient with a positive finding of suspected coagulopathy, which was subsequently discarded, with no intraoperative or postoperative complications observed in the series of studied cases; similar results were evidenced in a study of 56,000 surgeries, of which 5,120 were performed without preliminary studies and only with a normal clinical examination, showing that the patients were able to undergo anesthesia and surgery safely and with good intraoperative and postoperative results6. Another study of 169 adults undergoing herniorrhaphy concluded that it is rare for a normal history and physical examination to show perioperative bleeding, suggesting that routine preoperative testing in healthy patients is of little value9.
Despite the available evidence, the preoperative routine in many pediatric surgical centers includes a laboratory screening of hemostasis, the most requested tests are TP, APTT and hemogram, although we also observed tests such as bleeding time and clotting time; in our study of 69 routine studies we observed alteration in 21% of them, mainly in TP, however we did not observe intraoperative or postoperative bleeding complications, nor was any coagulation disorder diagnosed in children with altered tests. This is explained on the basis of the findings of a meta-analysis that evaluated 9 good quality observational studies, corroborating that coagulation tests have a low positive predictive value (0.03-0.22) and likelihood ratio (0.94-5.1) indicating that they are poor predictors of bleeding, and recommending that patients with a negative clinical history of bleeding do not require laboratory screening prior to surgery2.
The study also provides information on tests requested arbitrarily (non-routine) and on some measures taken into account to correct any altered results in routine tests; we observed that 149 tests (out of 218 tests) were requested non-routinely and without clinical justification, without providing any benefit in terms of clinical or surgical management; Similar results were analyzed in 2 studies in 520 patients undergoing non-cardiac surgery, which concluded that routine tests are neither useful nor cost-effective, recommending that they be requested only on the basis of concomitant diseases and the type of surgery to be performed5,7.
Something not described in similar literature is this practice of correcting values of some altered complementary test, without corroborating with the clinic, a practice identified in 18% of the patients and that includes from repeating and confirming the altered study to the transfusion of blood products, a very striking situation, because it could not only be considered useless and not cost-effective, but also risky because of the possible complications of the transfusion of hemoderivatives, which in these cases far outweigh the benefits; For the purposes of the study, the transfused patients were not followed up; however, none of them presented complications during their hospital stay.
The benefit of a laboratory screening for coagulation disorders with the tests is low, mainly because of its low sensitivity and specificity, as well as its low positive predictive value and likelyhood ratio2, in addition to this mention that coagulation disorders are rare diseases; in the HNMAV in 2018 of 55 000 patients attended 2 cases of hemophilia were diagnosed per year mainly by clinic, no other coagulopathies were diagnosed in that year.
Charges to patients amounted to 47 Bs per patient on a routine basis, and of 255 Bs per patient for charges associated with non-routine tests or intended for the correction of altered values in 15 patients; so on average a cost in preoperative laboratory tests of approximately 102 Bs per patient is disbursed.
If laboratory tests for all surgery outpatients or for minor procedures had been ordered according to the findings of the patient’s medical history and physical examination instead of by routine or arbitrary criteria, in 69 patients studied, laboratory tests were justified in only 1 case; therefore, our hospital could have potentially reduced patient costs by more than 7000 Bs. in the study group, and it can be inferred that during the period of one year it can be reduced between 32100 Bs. to 187 000 Bs. without expected adverse results.
In conclusion, the study established that routine preoperative screening tests have little utility and are not very cost-effective in the assessment of hemostasis for minor or outpatient procedures, compared to a clinical history and directed physical examination; their indication being appropriate when there are abnormal findings in the physical examination and clinical history or on the basis of concomitant diseases; Additional multicenter studies are required16 to extend the recommendations to other cities with the same geographic, sea level altitude and sociodemographic characteristics of our country, trying to guide medical behaviors to be more efficient with the use of resources, in a context of limited resources.
Conflict of interest: the authors declare that there is no conflict of interest.
References
1.Rapaport SI. Preoperative hemostatic evaluation: which tests, if any? Blood 1983.https://doi.org/10.1182/blood.V61.2.229.bloodjournal612229 [ Links ]
2. Chee YL, Crawford JC, Watson HG, Greaves M. Guidelines on the assessment of bleeding risk prior to surgery or invasive procedures. British Committee for Standards in Haematology. Br J Haematol 2008. https://doi.org/10.1111/j.1365-2141.2007.06968.x
3. Cosmi B, Alatri A, Cattaneo M, et al. Assessment of the risk of bleeding in patients undergoing surgery or invasive procedures: Guidelines of the Italian Society for Haemostasis and Thrombosis (SISET). Thromb Res 2009. https://doi.org/10.1016/j.thromres.2009.08.005
4. De Paepe A, Malfait F. Bleeding and bruising in patients with Ehlers-Danlos syndrome and other collagen vascular disorders. Br J Haematol 2004. https://doi.org/10.3109/9780203997352.078
5. Velanovich V. The value of routine preoperative laboratory testing in predicting postoperative complications: a multivariate analysis. Surgery 1991. [ Links ]
6. Narr BJ, Warner ME, Schroeder DR, Warner MA. Outcomes of patients with no laboratory assessment before anesthesia and a surgical procedure. Mayo Clin Proc 1997. https://doi.org/10.1016/S0002-9394(14)70851-7 [ Links ]
7. Velanovich V. Preoperative laboratory screening based on age, gender, and concomitant medical diseases. Surgery 1994. https://doi.org/10.1097/00132586-199410000-00026
8. Wattsman TA, Davies RS. The utility of preoperative laboratory testing in general surgery patients for outpatient procedures. Am Surg 1997. [ Links ]
9. Adams JG Jr, Weigelt JA, Poulos E. Usefulness of preoperative laboratory assessment of patients undergoing elective herniorrhaphy. Arch Surg 1992. https://doi.org/10.1001/archsurg.1992.01420070061012 [ Links ]
10. Silver D. What Routine Preoperative Tests for Bleeding Tendencies? JAMA 1976. [ Links ]
11. Eisenberg JM, Clarke JR, Sussman SA. Prothrombin and partial thromboplastin times as preoperative screening tests. Arch Surg 1982. https://doi.org/10.1001/archsurg.1982.01380250030007 [ Links ]
12. Kaplan EB, Sheiner LB, Boeckmann AJ, et al. The usefulness of preoperative laboratory screening. JAMA 1985. https://doi.org/10.1001/jama.1985.03350480084025 [ Links ]
13. Segal JB, Dzik WH, Transfusion Medicine/Hemostasis Clinical Trials Network. Paucity of studies to support that abnormal coagulation test results predict bleeding in the setting of invasive procedures: an evidence-based review. Transfusion 2005. https://doi.org/10.1111/j.1537-2995.2005.00546.x [ Links ]
14. Wahlberg T, Blombäck M, Hall P, Axelsson G. Application of indicators, predictors and diagnostic indices in coagulation disorders. I. Evaluation of a self-administered questionnaire with binary questions. Methods Inf Med 1980. https://doi.org/10.1055/s-0038-1635279. [ Links ]
15. Laine C, Williams SV, Wilson JF. In the clinic. Preoperative evaluation. Ann Intern Med 2009. https://doi.org/10.7326/0003-4819-151-1-200907070-01006. [ Links ]
16. Copana R, Melean LG. Hiponatremia en pacientes postoperados en el Hospital del Niño Manuel Ascencio Villarroel, Cochabamba, Bolivia. Gac Med Bol. 2014. [ Links ]

