Sporotrichosis: an unusual case report
Esporotricosis: presentación de un caso inusual
Gaceta Médica Boliviana, vol. 43, no. 1, 2020
Universidad Mayor de San Simón
Casos clinicos
Received: 05 December 2019
Accepted: 03 March 2020

Abstract: Sporotrichosis is a subcutaneous mycosis of chronic evolution that can affect humans and animals, caused by the Sporothrix schenckii complex, it is considered an occupational disease and its route of entry is through trauma, it is frequent in children and adolescents. We report the case of a 12-year-old adolescent girl with a clinical history of one year of evolution of facial dermatosis located in the left preauricular region, consisting of an erythematous, scaly, indurated plaque with well-defined borders, of not well identified causes. The diagnosis of fixed cutaneous sporotrichosis was confirmed by culture isolation and biopsy of the lesion. The patient was discharged with potassium iodide treatment for two months.
Keywords: cutaneous sporotrichosis, Sporothrix schenckii, potassium iodide.
Resumen: La esporotricosis es una micosis subcutánea de evolución crónica que puede afectar a humanos y animales, causada por el complejo Sporothrix schenckii, se considera un padecimiento ocupacional y su vía de entrada es a través de traumatismos, es frecuente en niños y adolescentes. Se comunica el caso de una adolescente de 12 años, con historia clínica de un año de evolución de causas no bien identificadas de dermatosis facial localizada en región pre-auricular izquierda, constituida por una placa eritematosa, escamosa, indurada, de bordes definidos. Se confirmó el diagnóstico de esporotricosis cutánea fija por el aislamiento en el cultivo y biopsia de lesión. La paciente fue dada de alta con tratamiento de yoduro de potasio durante dos meses.
Palabras clave: esporotricosis cutánea, Sporothrix schenckii, yoduro de potasio.
Sporotrichosis is a chronic subcutaneous granulomatous fungal infection caused by the dimorphic fungal species complex Sporothrix schenckii, a common saprophyte of soil, moss and plant detritus. The disease is endemic in regions with a tropical or subtropical climate and among personnel involved in agriculture or handling plant material. After traumatic implantation of the pathogen in the skin, the disease develops as fixed cutaneous, lymphocutaneous or disseminated cutaneous sporotrichosis affecting mainly the extremities in its classical forms1.
For diagnosis, the clinical and epidemiological history is important, but confirmation of the diagnosis is made by direct examination (asteroid bodies are observed) and culture (characteristic colonies are observed); other less commonly used studies are histopathological, serological and animal inoculation studies2.
Therapeutic management includes systemic antifungal agents (itraconazole, fluconazole) and local measures (thermotherapy). Terbinafine has been used in some patients with efficient results, but there are not enough clinical studies to recommend its application; potassium iodide is used in underdeveloped countries with good therapeutic results2, 3, 4.
We report a rare case of fixed facial cutaneous sporotrichosis, where clinical suspicion together with microbiological investigations helped to confirm the diagnosis and appropriate management.
Case presentation
A 12-year-old female student patient from the rural area of Caquiña in the Muñecas Province, La Paz, Bolivia, came to the Children’s Hospital “Dr. Ovidio Aliaga Uria” for consultation. The lesion in the left preauricular region started as a red papule that slowly grew in size and number. The patient did not report trauma, but she did report frequenting areas of large vegetation for recreation with her schoolmates. Physical examination revealed dermatosis in the facial region, left pre-auricular region with a lesion characterised by an erythematous, indurated plaque with well-defined borders measuring 10 x 7 cm, three solutions of continuity measuring approximately 2 cm in diameter with minimal non-purulent secretion and no evidence of bleeding, slightly painful on palpation, and no lymphadenopathy (Figure 1).

Samples were taken from the lesion for biopsy and mycological examination, which subsequently reported positive for sporotrichosis, confirming the diagnosis of fixed cutaneous sporotrichosis. The patient was treated with potassium iodide for two months with very good evolution and resolution of the case.
Discussion
The geographical distribution of this mycosis is universal, but it predominates in tropical and subtropical climates. In Bolivia there is no official report of cases of sporotrichosis, but it is one of the most common cutaneous mycoses referred to the Hospital del Niño, generally from tropical areas close to the city of La Paz, such as the Yungas5,6.
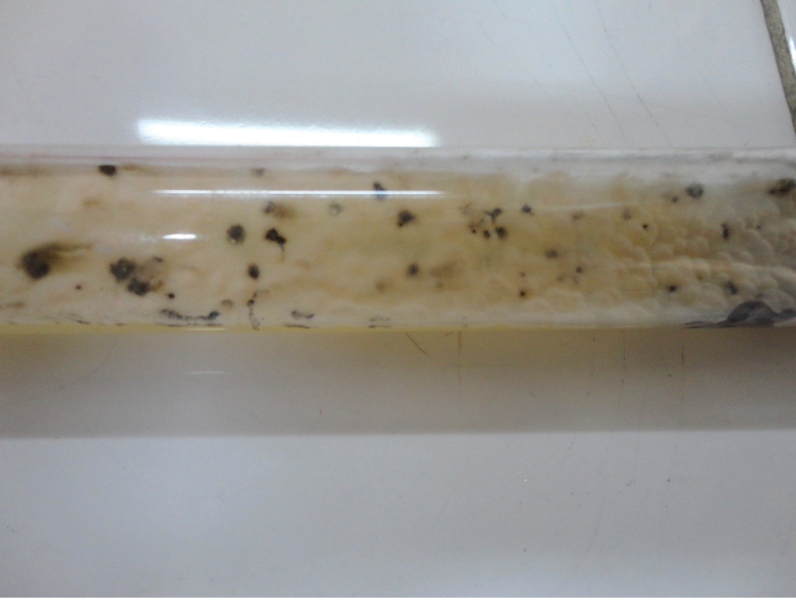
The patient came from a subtropical area of the department of La Paz, and presented lesions that were not so characteristic of sporotrichosis, so a precise diagnosis was not established at the time, and the following diseases were considered as differential diagnoses: chromomycosis and cutaneous tuberculosis, given the clinical characteristics of the lesions and the geographic antecedents, as well as the prolonged period of evolution. To confirm the diagnosis, the pathology laboratory was asked to perform a biopsy study of compromised tissue, which reported lesions compatible with sporotrichosis. The direct mycological examination and culture report revealed the presence of few yeasts in budding with narrow implantation. Samples obtained from the lesions were cultured by swabbing and secretion aspirate sown on Sabouraud’s medium with antibiotics at 25°C, where characteristic colonies were obtained between the third and sixth day, turning dark on the tenth day and almost black after 30 days (Figure 2)7 . Microscopic examination of these colonies revealed hyphae and conidia typical of Sporothrix schenckii, confirming the diagnosis of cutaneous sporotrichosis.
References
1. Chakrabarti A, Bonifaz A, Gutierrez-Galhardo MC, Mochizuki T, Li S. Global epidemiology of sporotrichosis. Med Mycol. 2015;53:3–14
2. Mahajan V.K. Sporotrichosis: an overview and therapeutic options. Dermatol. Res. Prac. 2014;2014:272376.
3. Kauffman C, Bustamante B, Chapman S, Pappas P. Clinical Practice Guidelines for the Management of Sporotrichosis: 2007 Update by the Infectious Diseases Society of America. IDSA Guidelines for Management of Sporotrichosis CID 2007;45:1255-65.
4. Bonifaz A, Vázquez D. Diagnosis and Treatment of Lymphocutaneous Sporotrichosis: What Are the Options?. Curr fungal infect rep 2013;7:252-9.
5. Rubio G, Sánchez G, Porras L, Alvarado Z. Esporotricosis: prevalencia, perfil clínico y epidemiológico en un centro de referencia en Colombia. Rev Iberoam Micol. 2010;27:75–9.
6. Michel da Rosa AC, Scroferneker ML, Vettorato R et al. Epidemiology of sporotrichosis: a study of 304 cases in Brazil. J Am Acad Dermatol 2005; 52:451-459. [ Links ]
7. De Araujo T, Marquez AC, Kerdel F. Sportrichosis. Int J Dermatol 2001;40:737-742.
Author notes
E-mail: dr.jpjaldin@gmail.com
Alternative link
http://www.scielo.org.bo/scielo.php?script=sci_arttext&pid=S1012-29662020000100016&lng=es&nrm=iso (html)

